Extended-Release vs. Immediate-Release Medications: When Timing Matters for Safety
 Nov, 24 2025
Nov, 24 2025
When you take a pill, you expect it to work. But not all pills work the same way. Some hit fast and hard. Others creep in slowly, like a tide rising over hours. The difference between extended-release and immediate-release medications isn’t just about convenience-it’s about safety, effectiveness, and sometimes, your life.
How These Two Types Actually Work
| Feature | Immediate-Release (IR) | Extended-Release (ER) |
|---|---|---|
| Time to peak effect | 30-90 minutes | 2-4 hours |
| Duration of effect | 4-8 hours | 12-24 hours |
| Dosing frequency | 3-4 times daily | 1-2 times daily |
| Peak concentration (Cmax) | High-can trigger side effects | Lower, more stable |
| Release mechanism | Simple dissolution in stomach | Matrix, osmotic pump, or coating |
Immediate-release pills are the classic kind. You swallow them, and within an hour, your body starts absorbing the full dose. That’s great if you need fast relief-like a painkiller for a sudden headache or an anxiety pill before a flight. But it also means your blood levels spike quickly, then drop just as fast. That rollercoaster can cause side effects: dizziness, nausea, jitteriness, or even seizures in extreme cases.
Extended-release pills are engineered differently. They don’t dump everything at once. Instead, they use smart systems-like a gel matrix that slowly dissolves, or a tiny pump that pushes the drug out over hours. Think of it like a slow drip from a faucet instead of turning it on full blast. Drugs like bupropion XR, metformin ER, or Adderall XR are built this way. The goal? Keep drug levels steady so you feel consistent relief without the highs and crashes.
Why Timing Changes Everything
It’s not just about how long the drug lasts. It’s about how your body reacts to the timing.
Take bupropion, used for depression and smoking cessation. The immediate-release version can spike blood levels to 600 ng/mL within two hours. That’s above the 350 ng/mL seizure risk threshold. The extended-release version? It holds steady at 100-200 ng/mL all day. That’s why you can safely take 300 mg of bupropion XR but never more than 150 mg of IR in a single dose.
Same goes for ADHD meds. Adderall IR lasts 4-6 hours, so kids often need a dose at school. Adderall XR lasts 10-12 hours. One pill in the morning covers the whole day. That’s less disruption, fewer stigma issues, and better focus. But here’s the catch: if you need a quick boost for a presentation or a big meeting, IR can be a lifesaver. That’s why some people keep a small IR dose on hand-just for emergencies.
And then there’s the flip side. If you’re on metoprolol ER for high blood pressure, you might not feel anything right away. That doesn’t mean it’s not working. It takes 7-10 days to reach steady state with ER meds, compared to 3-5 days with IR. A lot of people panic and take an extra pill because they “don’t feel it.” That’s how overdoses happen.
The Hidden Risks Nobody Talks About
Most people think ER pills are safer. And in many ways, they are. But they come with risks that IR doesn’t.
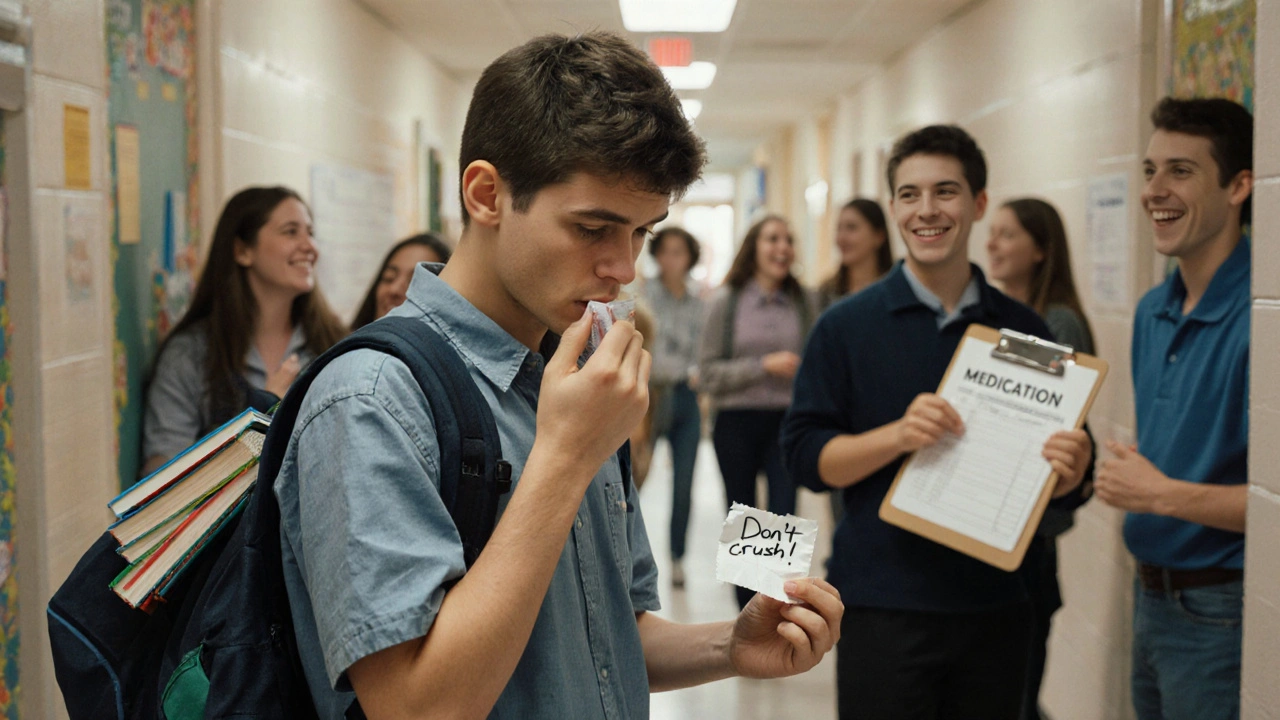
First: never crush, split, or chew an ER pill. The FDA warns this for nearly all extended-release products. If you break open a Concerta tablet or crush a Venlafaxine XR capsule, you’re releasing the entire dose at once. That’s not just ineffective-it’s dangerous. In 2020, the FDA issued a safety alert after multiple deaths from crushed extended-release opioids. People thought they were helping themselves by taking it faster. Instead, they got a lethal overdose.
Second: delayed onset can lead to accidental overdose. A 2022 GoodRx survey of 5,000 people found 41% didn’t understand ER meds take time to work. Nearly 30% took an extra dose because they felt nothing after an hour. Nine percent ended up in the ER with side effects from unintentional overdosing. That’s not just a mistake-it’s a systemic education failure.
Third: ER overdose is harder to treat. In a poisoning case, IR drugs clear from the body in 8-12 hours. ER drugs? They keep releasing for 24-48 hours. A 2021 National Poison Data System report showed ER bupropion overdoses required 2-3 times longer hospital stays than IR versions. Your body can’t flush it out fast enough. Doctors have to monitor you for days.
And here’s a sneaky one: your stomach matters. If you have gastroparesis-delayed stomach emptying-the ER pill can sit there too long and dump all at once. The FDA flagged this in July 2023. People with diabetes or Parkinson’s are especially at risk. Your doctor needs to know your full medical history before prescribing ER meds.
Who Should Use Which?
It’s not about which is “better.” It’s about which fits your life and condition.
Choose extended-release if:
- You’re managing a chronic condition like depression, hypertension, or ADHD
- You struggle to remember multiple daily doses
- You’ve had side effects from peaks and crashes with IR
- You want fewer fluctuations in mood or energy
Choose immediate-release if:
- You’re starting a new medication and need to titrate the dose
- You need quick relief for breakthrough symptoms (pain, anxiety, panic)
- You’re in a hospital or emergency setting where fast action matters
- You have digestive issues that affect absorption (like gastroparesis or Crohn’s)
For example, a patient with chronic depression might start on IR sertraline to find the right dose. Once stable, they switch to sertraline ER for smoother, all-day coverage. That’s not just common-it’s standard practice.
Cost, Compliance, and Real-World Trade-Offs
ER versions cost more. Adderall XR runs $350-$450 for 30 pills. The IR version? $280-$380. That’s a 15-25% premium. But here’s the twist: people on ER meds are 22% more likely to stick with their treatment.
A 2022 JAMA study tracked 15,000 people with high blood pressure. Those on ER versions had 78% adherence over 12 months. Those on IR? Only 56%. That’s not just about forgetting pills-it’s about how the medication feels. If you’re not crashing by 3 p.m. or waking up jittery, you’re more likely to keep taking it.
And it’s not just numbers. On Reddit’s ADHD community, users consistently say ER gives them a “smooth ride.” One wrote: “I used to have a 2 p.m. crash with IR. Now I just work. No spikes, no crashes.” That’s the real win.
But don’t ignore the downside. If you’re trying to manage acute anxiety or need to adjust your dose quickly, ER can feel like a trap. You’re stuck waiting for something that won’t kick in fast enough. That’s why doctors keep IR options on the table-even if they prefer ER for maintenance.

What to Do Next
If you’re on an ER medication:
- Read the label. If it says “do not crush, chew, or split,” don’t. Even if the pill is big or hard to swallow.
- Wait at least 4 hours before taking another dose. If you don’t feel anything, it doesn’t mean it’s not working.
- Talk to your pharmacist. Ask: “Is this ER? How long until it starts? What happens if I miss a dose?”
- Keep a log. Note when you take it, when you feel effects, and any side effects. That helps your doctor adjust things safely.
If you’re considering switching from IR to ER:
- Don’t switch cold turkey. Your doctor needs to taper you down first.
- Give it time. It can take up to 10 days to feel the full benefit.
- Ask if there’s a generic version. Many ER drugs now have affordable generics.
And if you’re on IR:
- Set alarms. Use your phone to remind you when to take your next dose.
- Don’t double up if you miss one. Wait until your next scheduled time.
- Keep a small emergency dose if you need fast relief-but only if your doctor says it’s safe.
Bottom Line
Extended-release and immediate-release aren’t better or worse. They’re different tools for different jobs. One gives you speed. The other gives you stability. The problem isn’t the pill-it’s the misunderstanding around it.
Too many people think ER is just a “stronger” version of IR. It’s not. It’s a different delivery system. Misuse it, and you risk serious harm. Use it right, and it can transform your life.
Ask your doctor: “Is this ER or IR? Why? What happens if I take it wrong?” That one conversation could prevent an emergency.
Can I split an extended-release pill in half?
No-unless the pill has a score line and your doctor or pharmacist specifically says it’s safe. Most extended-release pills, like Concerta or Venlafaxine XR, are designed to release medication slowly over time. Splitting, crushing, or chewing them releases the full dose all at once, which can cause dangerous spikes in drug levels. Even pills that look easy to split may have hidden coatings or matrices that are destroyed when broken. Always check the label or ask your pharmacist before altering any pill.
Why don’t I feel anything after taking my ER medication?
Extended-release medications are designed to work slowly. It can take 2-4 hours to reach therapeutic levels, and up to 7-10 days to reach full steady-state effectiveness. If you’re taking it for depression, high blood pressure, or ADHD, you won’t feel an immediate “high” or “rush.” That’s normal. Taking an extra dose because you don’t feel anything right away is one of the most common causes of accidental overdose with ER drugs. Stick to your schedule and give it time.
Is extended-release always better than immediate-release?
No. Extended-release is better for long-term, stable conditions like chronic depression, hypertension, or ADHD maintenance. But immediate-release is essential for titrating doses, treating breakthrough symptoms (like sudden pain or panic attacks), or in emergency settings. For example, someone on bupropion XR might keep a low-dose IR tablet on hand for acute focus needs. The right choice depends on your condition, lifestyle, and how your body responds.
What should I do if I accidentally crush or chew an ER pill?
Call your doctor or poison control immediately. Even if you feel fine, the full dose may be entering your system faster than intended. For drugs like opioids or bupropion, this can lead to respiratory depression, seizures, or heart rhythm problems. Do not wait for symptoms to appear. ER pills are designed to release slowly-breaking that system can be life-threatening.
Can I switch from IR to ER on my own?
Never. Switching between immediate-release and extended-release formulations requires medical supervision. The dosing isn’t always 1:1. For example, 30 mg of Adderall IR is not the same as 30 mg of Adderall XR in how it’s absorbed over time. Your doctor needs to adjust the dose and monitor you for side effects. Going from IR to ER without guidance can lead to underdosing, overdosing, or withdrawal symptoms.
Are ER medications more expensive? Is it worth it?
Yes, ER versions often cost 15-25% more than IR. But they can save you money in the long run. Studies show patients on ER meds are 22% more likely to take them consistently, reducing hospital visits and emergency care. For chronic conditions, better adherence means fewer complications-like strokes from uncontrolled blood pressure or depressive episodes from missed doses. If cost is an issue, ask about generic ER options. Many are now available and just as effective.
What to Watch For Next
The future of medication delivery is changing. Researchers are testing 3D-printed pills that release different drugs at exact times-like a mini pharmacy in one tablet. New ER systems are being built to resist abuse, turning into gel when crushed. But the basics haven’t changed: timing matters. Safety matters. And understanding how your pill works is still the most powerful tool you have.

katia dagenais
November 25, 2025 AT 23:53Okay but have you ever tried crushing an ER pill just to see what happens? I did. It was like a chemical fireworks show in my brain. Not recommended. Also why do people think slow release means weak? It’s not about intensity-it’s about harmony. Your body isn’t a car that needs to rev to 8k RPM every morning.
Josh Gonzales
November 26, 2025 AT 04:34ER meds save lives but nobody teaches you how to use them. My dad took his metoprolol ER and thought it wasn’t working so he doubled up. Ended up in the ER with a heart rate of 42. He’s fine now but he still doesn’t get why waiting 4 hours matters. We need better patient education like yesterday.
Jack Riley
November 26, 2025 AT 20:37Let’s be real-extended-release isn’t magic. It’s just capitalism in pill form. Companies make more money off a 30-day supply that costs $400 instead of three 10-day IR packs at $120. And yes, adherence is higher-but is that because people love the drug or because they’re too scared to risk missing a dose and crashing? We’re medicating compliance, not health. The real issue? We treat patients like broken machines that need perfect timing to function. What if the problem isn’t the pill but the expectation that we should feel ‘normal’ every single day? Maybe we need less control and more acceptance of human rhythm. Also I once chewed a Concerta because I was late for class. I cried for three hours. Worth it.
Jacqueline Aslet
November 27, 2025 AT 21:26It is, indeed, a matter of considerable concern that the general populace remains profoundly uninformed regarding the pharmacokinetic distinctions between immediate-release and extended-release pharmaceutical formulations. The consequences of improper administration, as elucidated in the aforementioned text, are not merely clinical-they are existential. One must question the integrity of modern medical education when laypersons believe that a tablet’s physical manipulation is a trivial act. The FDA’s warnings are not suggestions. They are lifelines.
Caroline Marchetta
November 28, 2025 AT 16:10So let me get this straight… you’re telling me the reason I felt like a zombie for two weeks after switching to ER sertraline is because ‘it takes 10 days’? But my doctor didn’t warn me. And now I’m on a 100mg dose because ‘the ER version is smoother’-except I feel like I’m underwater during a thunderstorm. Who’s really responsible here? The pill? Or the system that sells us slow-release hope while ignoring the fact that some of us just need to feel alive now?
Valérie Siébert
November 30, 2025 AT 09:20ER is a game changer for ADHD. No more lunchtime pill panic. No more teacher side-eye. I used to have to go to the nurse every day and now I just take one in the morning and boom-focus for 12 hours. Also side note: if you think ER means you can skip meals, you’re wrong. I learned that the hard way. My stomach hated me for a week. But still worth it.
Ellen Sales
December 1, 2025 AT 04:50THIS. This right here. I’ve been on bupropion ER for 3 years and I never knew about the gastroparesis risk. My cousin has diabetes and she was on it for months before her doctor even asked about digestion. I’m telling everyone I know. Please, if you’re on ER meds, talk to your pharmacist. They’re the real heroes. Also-don’t crush pills. I mean it. I’ve seen what happens. It’s not pretty.
Josh Zubkoff
December 1, 2025 AT 18:28Look, I get it. Extended-release sounds fancy. But let’s be honest-this whole post reads like a pharmaceutical ad written by someone who’s never had to take a pill at 2 a.m. because their kid is screaming and their partner is asleep and they’re just trying to survive. The ‘smooth ride’ people talk about? That’s for people who have time, money, and a support system. What about the single mom working two jobs who forgets to take her med because her alarm didn’t go off? You think she’s gonna read the label? She’s gonna take half a pill because she thinks ‘more is better’ and then she ends up in the ER and the system blames her for not being educated enough. Meanwhile the drug company makes a profit. That’s not safety. That’s exploitation dressed up as science.
fiona collins
December 2, 2025 AT 08:28Thank you for this clear, vital breakdown. I’ve shared it with my clinic’s patient handouts.
Andrew McAfee
December 3, 2025 AT 22:09Man I used to take Adderall IR in college and it was a mess. One pill at 8am, another at 1pm, another at 5pm. I was always counting pills like a drug dealer. Then I switched to XR and it felt like I got my life back. No more hiding in the bathroom to swallow pills. No more panic when I missed one. Just… calm. I’m not saying it’s perfect but it’s better. Also-never crush. I saw a guy do it once. He screamed for 45 minutes. We called 911. He lived. But dude, don’t do it.
Erika Hunt
December 5, 2025 AT 05:59I’m a nurse and I see this every week. Someone comes in because they took their ER oxycodone after crushing it because they were in pain and thought ‘it’ll work faster.’ They don’t understand that the coating isn’t just there to make it pretty-it’s there to keep them alive. And then they get mad when we say ‘you shouldn’t have done that.’ Like we’re the bad guys. We’re just trying to stop you from dying. I wish we could hand out these explanations with every prescription. Not just the label. The real talk. The kind that doesn’t sound like a textbook. The kind that says: ‘Your body isn’t a vending machine. Don’t shake it.’