Aspirin Therapy for Heart Disease Prevention: Who Really Needs It in 2026?
 Jan, 3 2026
Jan, 3 2026
Aspirin isn't the magic shield for heart attacks you think it is
For decades, popping a baby aspirin every morning was common advice - especially if you had a family history of heart disease. Your grandparent did it. Your neighbor still does it. But here’s the truth: aspirin therapy for preventing a first heart attack or stroke is no longer recommended for most people. Not because it doesn’t work, but because the risks now often outweigh the benefits - especially if you’re over 60 or don’t have existing heart disease.
Back in the 1980s, studies like the Physicians’ Health Study showed aspirin could cut heart attack risk in half for middle-aged men. That led to a global surge in daily aspirin use. But those studies were done before statins, before blood pressure meds were as effective, before we understood how common bleeding risks really are. Today, the science has flipped. Major health groups like the U.S. Preventive Services Task Force (USPSTF) and the American Heart Association now say: don’t start aspirin for prevention unless your doctor specifically tells you to.
Who might still benefit from aspirin therapy?
It’s not a blanket no. There’s a narrow group where the math still works. If you’re between 40 and 59, and your 10-year risk of heart disease is 10% or higher, aspirin might be worth considering - but only after a deep conversation with your doctor.
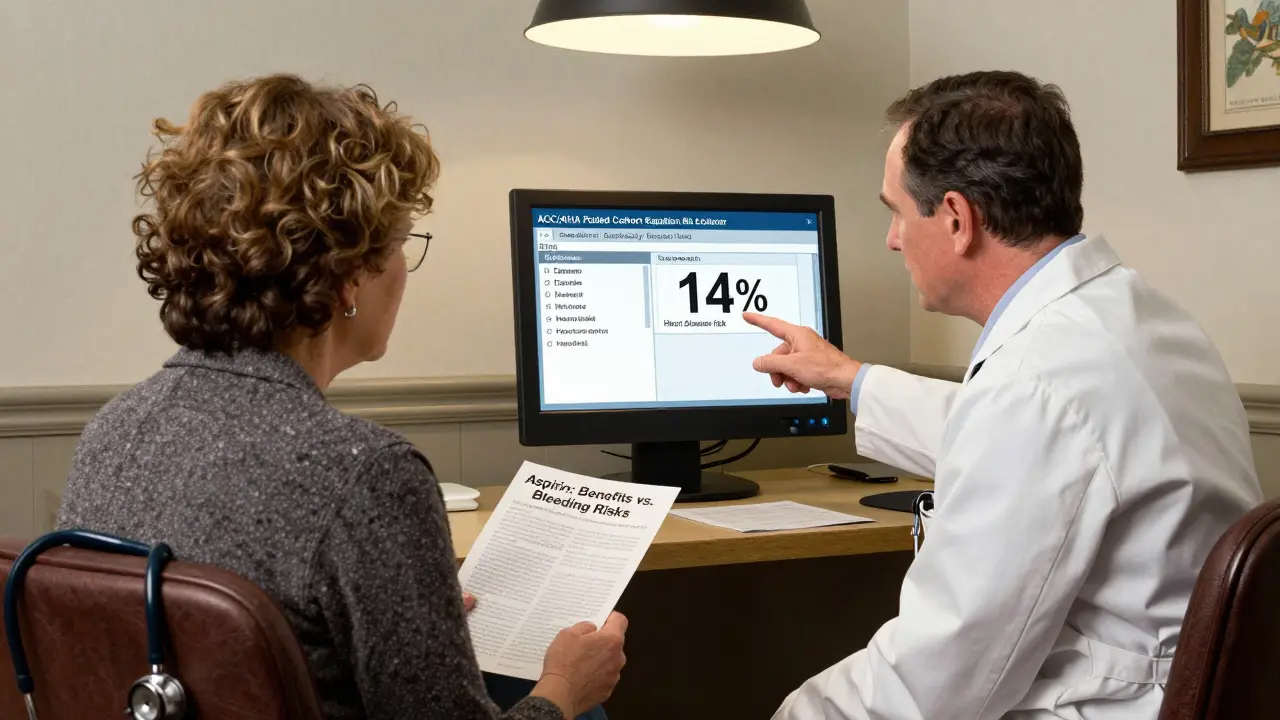
How do you know your 10-year risk? It’s calculated using your age, sex, race, blood pressure, cholesterol levels, diabetes status, and whether you smoke. This isn’t guesswork. Doctors use the ACC/AHA Pooled Cohort Equation, built into most electronic medical records. If you’re a 52-year-old man with high LDL cholesterol, untreated high blood pressure, and you smoke, your risk might be 14%. In that case, aspirin’s small benefit - reducing nonfatal heart attacks by about 10% over 10 years - could make sense.
But here’s the catch: if you have even one bleeding risk factor, it’s probably not worth it. That includes:
- A history of stomach ulcers or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Heavy alcohol use (more than 3 drinks a day)
- Age 60 or older
- Kidney or liver disease
People with diabetes are a special case. The American Diabetes Association still says aspirin can be considered for those over 40 with additional risk factors - like high blood pressure or smoking - because their heart disease risk is naturally higher. But even then, it’s not automatic. Some endocrinologists now skip aspirin entirely and focus on tighter glucose control and statins instead.
Why aspirin’s benefit has shrunk so much
Think of aspirin as a blunt tool. It stops blood clots by making platelets less sticky. That helps if you already have clogged arteries - which is why it’s a lifesaver after a heart attack or stroke. But for someone with healthy arteries? The benefit is tiny.
Modern medicine has changed the game. Statins lower LDL cholesterol by 30-50%, cutting heart attack risk by 25-37%. Blood pressure meds bring systolic pressure down from 150 to 120, slashing stroke risk. We now have better tools than aspirin for primary prevention. As Dr. Erin Michos from Johns Hopkins put it: “With better control of traditional risk factors, aspirin’s benefit has shrunk to almost nothing.”
Meanwhile, the bleeding risk hasn’t gone down. Every year, for every 100 people taking low-dose aspirin (75-100 mg) for primary prevention, about 1 will avoid a heart attack - but 2 will have a major bleeding event. That’s not a trade-off most people would choose if they understood it.
The bleeding risk is real - and often ignored
Most people think aspirin is harmless. It’s cheap. It’s over the counter. But it’s a drug. And like any drug, it can cause serious harm.
Major bleeding includes:
- Stomach or intestinal bleeding (can lead to anemia or hospitalization)
- Brain hemorrhages (stroke caused by bleeding, not clotting)
- Severe nosebleeds requiring medical attention
One 2019 study found aspirin increases the risk of major bleeding by 43%. For someone over 70, that risk jumps even higher. A 2022 JAMA Internal Medicine study warned that continuing aspirin for primary prevention in adults over 70 may cause more harm than all motor vehicle accidents combined in that age group.
And here’s the scary part: many people don’t even know they’re at risk. A 2019 Circulation study found 6.6 million Americans take aspirin daily for prevention without ever talking to a doctor. They’re doing it based on habit, family history, or a 10-year-old recommendation.
What about family history? Does that matter?
It’s the most common reason people cling to aspirin. “My dad had a heart attack at 58 - I need to take it.” But family history alone isn’t enough to justify daily aspirin. If you have a strong family history, your doctor should focus on aggressive risk factor control: statins, exercise, quitting smoking, managing blood pressure - not aspirin.
There’s one exception: familial hypercholesterolemia. That’s a genetic condition where LDL cholesterol is sky-high from birth. People with this condition often have heart disease risk equivalent to someone 20 years older. For them, aspirin may still be considered - but only after lipid specialists review their full profile.
For everyone else, family history just means you need to be more vigilant about lifestyle and medication - not that you need aspirin.
Aspirin still saves lives - but only after a heart event
Don’t confuse primary and secondary prevention. If you’ve already had a heart attack, stroke, stent, or bypass surgery, aspirin is still a cornerstone of treatment. In secondary prevention, it cuts the risk of another event by 21% and lowers death risk by 13%. That’s why millions of people with existing heart disease take it daily - and that’s not changing.
The confusion comes when people who’ve never had a heart problem assume they need it too. They don’t. If you’re healthy, your best defense isn’t a pill. It’s walking 30 minutes a day, eating more vegetables, sleeping well, and managing stress. Those things cut heart disease risk more than aspirin ever could.
What should you do if you’re already taking aspirin?
If you’re over 60 and taking aspirin for prevention - stop. Don’t quit cold turkey, but talk to your doctor. They’ll help you taper safely if needed. Many people who stop report fewer nosebleeds, less bruising, and better digestion.
If you’re under 60 and have no heart disease, ask your doctor to calculate your 10-year risk. If it’s below 10%, aspirin isn’t helping you. If it’s above 10%, ask: “What are my bleeding risks?” and “Are statins or blood pressure meds a better first step?”
And if you’re 40-59 with no known risk factors? Don’t start. The evidence shows no net benefit for healthy people in this age group.

Alternatives to aspirin for heart health
If you’re looking to prevent heart disease, aspirin isn’t your best bet. Here’s what actually works:
- Statins - Lower LDL cholesterol, reduce inflammation in arteries. Most effective for primary prevention.
- Blood pressure control - Keeping systolic pressure under 120 cuts stroke risk dramatically.
- Regular exercise - 150 minutes of moderate activity a week reduces heart disease risk by 30%.
- Healthy diet - Mediterranean-style eating (olive oil, nuts, fish, veggies) is proven to protect the heart.
- Quitting smoking - One of the single biggest wins for heart health.
These aren’t just “good ideas.” They’re backed by decades of data. And unlike aspirin, they don’t come with a 43% higher risk of internal bleeding.
Why are so many people still taking aspirin?
Because old habits die hard. And because doctors - even good ones - sometimes keep prescribing it out of caution or because patients ask for it.
A 2021 study found only 43% of primary care doctors could correctly calculate a patient’s 10-year heart disease risk. Many still rely on intuition or family history. Meanwhile, patients hear “aspirin prevents heart attacks” from TV ads or their parents and assume it’s safe.
The Veterans Health Administration ran a program to stop inappropriate aspirin use - and cut it by 37% in three years. That shows change is possible. But in private practices, aspirin prescriptions for primary prevention are still 20-25% higher than guidelines recommend.
It’s not about blame. It’s about awareness. We’ve moved past the era of one-size-fits-all prevention. Today, heart health is personal.
Final takeaway: Aspirin is not a daily vitamin
Aspirin isn’t harmless. It’s not a supplement. It’s a powerful drug with real, measurable risks. For people with no heart disease, the benefits are small - and fading. For people over 60, the risks are growing.
If you’ve never had a heart attack or stroke, and you’re taking aspirin daily - talk to your doctor. Don’t assume it’s helping you. Ask: “What’s my actual risk? What’s my bleeding risk? Is this still right for me?”
The best heart health strategy isn’t a pill you swallow every morning. It’s a conversation you have with your doctor - and a lifestyle you choose every day.
Should I take aspirin every day to prevent a heart attack?
No, not if you haven’t had a heart attack, stroke, or stent. For most people without existing heart disease, daily aspirin does more harm than good. The risk of serious bleeding - especially in people over 60 - outweighs the small chance of preventing a first heart event. Only consider it if you’re 40-59 with high heart disease risk and low bleeding risk, and only after talking to your doctor.
Is baby aspirin safer than regular aspirin?
The dose matters more than the label. “Baby aspirin” usually means 75-100 mg, which is the only dose studied for prevention. But even low-dose aspirin carries the same bleeding risks as higher doses. There’s no “safe” version for people without heart disease. The problem isn’t the dose - it’s taking it at all when you don’t need it.
Can I take aspirin if I have diabetes?
It’s possible, but not automatic. The American Diabetes Association says aspirin can be considered for people with diabetes over 40 who have other risk factors like high blood pressure or smoking. But many experts now prefer statins and tighter glucose control instead. Always get your 10-year heart disease risk calculated before deciding.
What if my doctor told me to take aspirin - should I still stop?
Ask why. Many doctors still prescribe aspirin based on outdated advice or patient pressure. Request a risk calculation using the ACC/AHA Pooled Cohort Equation. If your 10-year risk is below 10%, or you’re over 60, the guidelines say not to start. If you’re already taking it, discuss stopping - especially if you have any bleeding risk factors.
Are there better alternatives to aspirin for heart health?
Yes. Statins are far more effective for preventing first heart events in most people. Blood pressure control, regular exercise, quitting smoking, and eating a Mediterranean-style diet have stronger evidence than aspirin - and no bleeding risk. Focus on these first. Aspirin should never be your primary tool for prevention.

Jacob Milano
January 4, 2026 AT 00:22Enrique González
January 4, 2026 AT 21:41Shanna Sung
January 6, 2026 AT 04:32John Ross
January 7, 2026 AT 12:18Ashley Viñas
January 8, 2026 AT 19:33Brendan F. Cochran
January 10, 2026 AT 01:01jigisha Patel
January 10, 2026 AT 06:13Justin Lowans
January 12, 2026 AT 01:04Michael Rudge
January 13, 2026 AT 01:31