Evergreening: How Pharmaceutical Brands Stretch Patents to Block Generic Drugs
 Dec, 9 2025
Dec, 9 2025
Every year, billions of dollars in drug sales hang on a single number: the expiration date of a patent. When that date passes, generic versions flood the market, prices drop by up to 85%, and patients finally get affordable access. But for many blockbuster drugs, that expiration date never really comes. Instead, companies use a legal maneuver called evergreening to keep generics out-long after the original patent should have expired.
What Evergreening Really Means
Evergreening isn’t about inventing new medicines. It’s about making tiny changes to old ones and filing new patents on those changes. Think of it like swapping out the battery in your phone and calling it a new model. The core function hasn’t changed, but now you get another 20 years of exclusive rights. This isn’t some shady loophole-it’s built into the system. The 1984 Hatch-Waxman Act in the U.S. was meant to balance innovation with access. It gave brand-name drugmakers 20 years of patent protection, but also created a faster path for generics. The problem? Companies quickly learned how to game the rules. Instead of developing new drugs, they started extending the life of existing ones. Take AstraZeneca’s Prilosec, a heartburn drug. When its patent was set to expire, the company launched Nexium-a slightly different version of the same molecule. Nexium wasn’t more effective. It didn’t work better for more people. But it had a new patent. And that patent delayed generics for over a decade. The result? Billions in extra revenue, while patients paid more for nearly the same pill.The Playbook: How Companies Extend Patents
There’s no single way to evergreen a drug. There are dozens. Here are the most common tactics:- New dosage forms: Switching from a pill to a capsule, liquid, or patch. Even if the active ingredient is identical.
- Combination products: Adding another drug to the mix-even if that second drug is old and off-patent. The combo gets a new patent.
- Extended-release versions: Making the drug last longer in the body. Often, this doesn’t improve outcomes, just changes how often you take it.
- Patent thickets: Filing dozens, even hundreds, of patents around one drug. AbbVie filed 247 patents on Humira, a drug for autoimmune diseases. Even if most are weak, the cost of fighting them deters generics.
- Product hopping: Pulling the original drug off the market while pushing the new version. Patients and doctors get nudged toward the new patent-protected version, even if it’s not better.
- Orphan drug designation: Repurposing a common drug for a rare disease to get seven years of exclusivity.
- Pediatric exclusivity: Running small studies on children to earn six extra months of protection.
Why This Matters for Patients
When generics enter the market, prices drop fast. Humira, for example, cost over $70,000 a year in the U.S. before generics. Now, with competition, it’s under $10,000. That’s life-changing for patients with rheumatoid arthritis, Crohn’s disease, or psoriasis. But evergreening delays that drop. In some cases, it delays it for over a decade. During that time, patients pay hundreds or thousands of dollars a month. Some skip doses. Some go without. Some go bankrupt. A 2023 study found that 78% of new patents on prescription drugs were for existing drugs-not new ones. That means most patent activity isn’t about innovation. It’s about profit. And it’s not just the U.S. The World Health Organization calls evergreening a major barrier to affordable medicines in low- and middle-income countries. When a drug like insulin or HIV medication is locked behind patent thickets, people die because they can’t afford it.
The Cost of Evergreening-For Everyone
Developing a truly new drug costs about $2.6 billion and takes 10 to 15 years. Evergreening? It costs a fraction of that. A few million dollars for a new formulation, a small clinical trial, and a team of patent lawyers. The return? Massive. AstraZeneca extended patent life on six drugs by more than 90 years combined. AbbVie made over $40 million a day from Humira during its patent monopoly. That’s not innovation. That’s rent-seeking. And the cost doesn’t stop at patient wallets. Insurance companies pay more. Medicare pays more. Governments pay more. The entire healthcare system bears the burden. Meanwhile, real innovation stalls. Why spend billions and a decade on a risky new drug when you can tweak an old one and lock in profits for years?Who’s Fighting Back?
There’s growing pushback. In 2022, the U.S. Federal Trade Commission sued AbbVie over Humira’s patent strategy, calling it anticompetitive. Courts are starting to question whether minor changes deserve patent protection. The European Medicines Agency now requires proof of real clinical benefit for new formulations. The Inflation Reduction Act of 2022 lets Medicare negotiate prices for the most expensive drugs. That cuts the profit motive behind evergreening. If the government won’t pay $70,000 for a drug, companies have less incentive to stretch patents. Some generic manufacturers are fighting back too. They’re challenging patent clusters in court. It’s expensive and slow-but it’s working. In 2023, a court ruled against a patent on a version of the asthma drug Advair, opening the door for generics.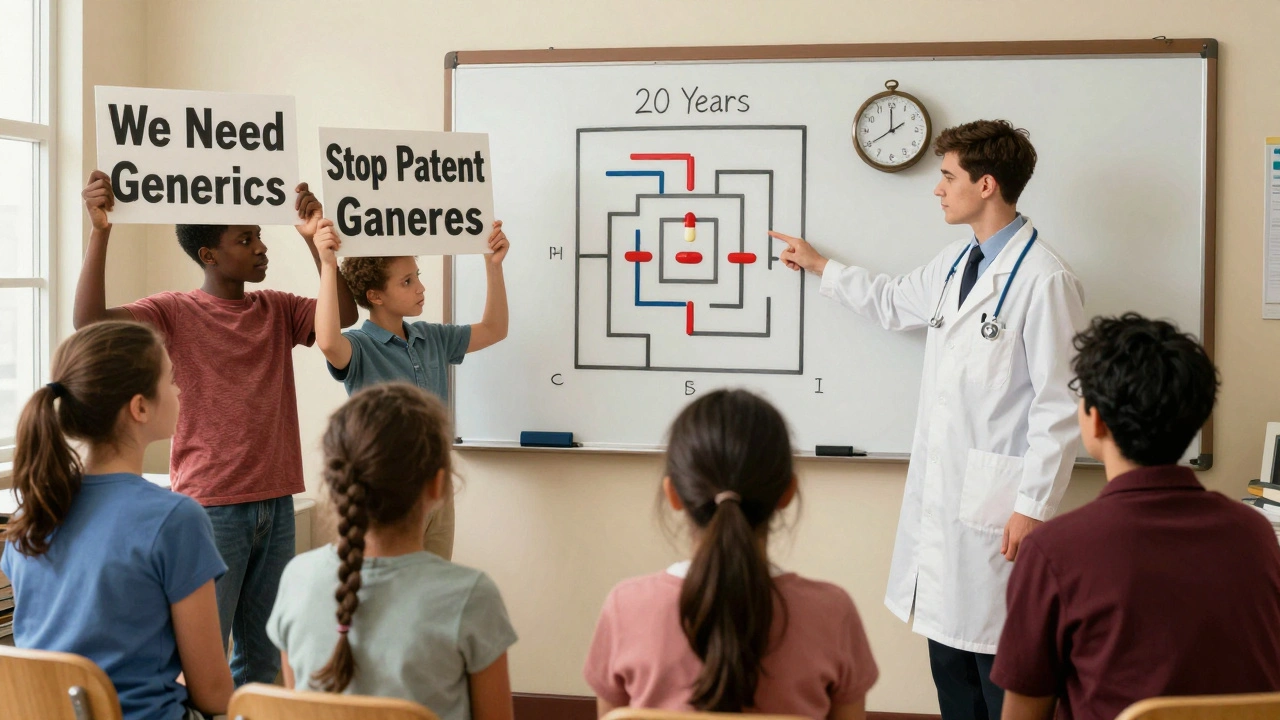
What’s Next?
Companies aren’t giving up. They’re just getting smarter. Now they’re moving into biologics-complex drugs made from living cells. These are harder to copy. Nanotechnology and pharmacogenomics (testing genes to predict drug response) are the next frontiers. Patenting a genetic test that says a patient will respond to a drug? That’s the new frontier. But the tide is turning. Public pressure is rising. Politicians are talking. Courts are listening. And patients are demanding change. The question isn’t whether evergreening will end. It’s how fast. Right now, the system rewards companies for delaying competition. The real innovation will come when it rewards them for creating drugs that actually help people-instead of just extending profits.How to Spot Evergreening in Your Own Prescription
If you’re on a brand-name drug and notice:- Your pharmacy suddenly stopped carrying the old version
- Your doctor switched you to a new form of the same drug
- You’re being told the new version is ‘better’ but can’t explain how
- The price didn’t drop even though the drug is old
Is evergreening legal?
Yes, it’s currently legal in the U.S. and many other countries. The patent system allows companies to file new patents for minor changes to existing drugs-even if those changes don’t improve effectiveness. Courts and regulators are starting to challenge these patents, but they’re still being granted. What’s legal isn’t always fair.
Do evergreened drugs work better than generics?
Almost never. Studies show that most evergreened versions-like Nexium, Suboxone, or extended-release Adderall-are no more effective than the original or the generic. The differences are often in how the drug is delivered, not how it works. Patients pay more for the same medicine.
How long can a drug stay protected through evergreening?
There’s no hard limit. AstraZeneca extended patent life on six drugs by over 90 years combined. AbbVie’s Humira could stay protected until 2034 thanks to over 247 patents. The original 20-year patent is just the start. With every new patent, the clock resets.
Can I get a cheaper version if my drug is evergreened?
Not until the last patent expires. Until then, generics can’t legally enter the market. Some patients use international pharmacies or patient assistance programs to get lower prices. But those aren’t reliable solutions. The real fix is ending the patent strategies that block generics.
Are there any drugs that haven’t been evergreened?
Most blockbuster drugs have been. The top 20 selling drugs in the U.S. all have multiple patents. Even older drugs like insulin, metformin, and aspirin have been reformulated and re-patented. Truly generic drugs-like those with no patent extensions-are now the exception, not the rule.
What’s being done to stop evergreening?
The U.S. FTC is suing companies like AbbVie. The FDA is tightening review standards. The EU requires proof of clinical benefit for new formulations. The Inflation Reduction Act lets Medicare negotiate prices, reducing the financial incentive. But progress is slow. The system still favors big pharma over patients.
What You Can Do
You don’t have to accept this system. Here’s how to push back:- Ask your doctor if a generic version is available.
- Check GoodRx or other price-comparison tools before filling prescriptions.
- Support policy changes that limit patent extensions and require proof of real benefit.
- Share stories about drug costs. Public pressure drives change.

Evelyn Pastrana
December 10, 2025 AT 03:51At this point, Big Pharma isn’t selling medicine. They’re selling a subscription to a rigged game.
Lisa Whitesel
December 10, 2025 AT 04:20Simran Chettiar
December 10, 2025 AT 17:42Richard Eite
December 10, 2025 AT 22:59Katherine Chan
December 12, 2025 AT 08:22Philippa Barraclough
December 12, 2025 AT 18:25Tim Tinh
December 13, 2025 AT 16:41Ruth Witte
December 13, 2025 AT 16:59WE NEED TO CALL THIS OUT. NO MORE BS. GIVE US THE GENERIC. I’M NOT PAYING FOR A NEW COLOR CAPSULE.
Katherine Rodgers
December 14, 2025 AT 00:43Lauren Dare
December 15, 2025 AT 06:47Lola Bchoudi
December 16, 2025 AT 18:12