How Manic-Depressive Disorder Affects Marriage and Intimate Relationships
 Nov, 18 2025
Nov, 18 2025
When someone in a marriage has manic-depressive disorder-now more commonly called bipolar disorder-the quiet moments between partners can become battlegrounds. Not because of lack of love, but because the illness doesn’t care how much you care. It flips the emotional switch without warning, turning tenderness into rage, devotion into detachment, and shared dreams into silent nights spent staring at the ceiling.
The Two Sides of the Same Coin
Bipolar disorder isn’t just mood swings. It’s extreme highs-manic episodes where sleep disappears, money flies out the door, and grand plans are made with no plan to finish them-and crushing lows where getting out of bed feels like climbing a mountain made of lead. These aren’t temporary bad days. They’re neurological events that alter perception, judgment, and emotional control.In a relationship, this means your partner might spend three weeks planning a business trip to start a new company, then cancel everything, lock themselves in the bedroom for a week, and refuse to speak. One month they’re the life of the party, buying gifts and planning vacations. The next, they’re convinced you’re cheating, even when there’s zero evidence. The inconsistency isn’t personal-it’s biological. But that doesn’t make it easier to live with.
Trust Erodes Without Warning
Trust in marriage is built on predictability. You expect your partner to show up. To keep promises. To be there when you need them. With bipolar disorder, those expectations get shattered. A partner might promise to attend your parent’s birthday, then vanish for days during a manic phase. Or they might accuse you of lying during a depressive episode, even after you’ve shown proof over and over.Studies from the National Institute of Mental Health show that nearly 70% of people with bipolar disorder report serious relationship conflicts within the first five years of marriage. The most common triggers? Financial recklessness during mania, emotional withdrawal during depression, and explosive arguments fueled by irritability.
One woman in Brisbane told me her husband spent $28,000 in six weeks on online gambling during a manic episode. He didn’t remember it. She didn’t know how to bring it up without triggering another episode. They separated for nine months. When he got stable on medication, he cried and asked if she’d ever forgive him. She did-but the trust never fully came back.
Intimacy Turns Into a Chore
Sexual desire doesn’t follow logic. During mania, some people become hypersexual-seeking out attention, flirting excessively, even having affairs. During depression, the same person might lose all interest in physical contact. Hugs feel like burdens. Kissing feels like work.One man I spoke with said his wife stopped initiating intimacy for 14 months because she was afraid of rejection. When she finally asked him why he never touched her, he said, “I thought you didn’t want me anymore.” Neither of them realized the other was waiting for permission to feel close again.
Physical closeness becomes a minefield. One partner wants connection. The other is either too overwhelmed or too detached to respond. Over time, that distance builds walls. And walls don’t break down with love alone-they need structure, patience, and sometimes professional help.

The Silent Burden on the Non-Bipolar Partner
Most people don’t talk about the toll on the partner who doesn’t have bipolar disorder. They’re not the patient. But they’re the one holding everything together. They manage bills after a spending spree. They drive to therapy appointments. They learn to read facial expressions to guess if today is a good day or a day they’ll need to leave the room.They stop sharing their own struggles. Why? Because their partner is already drowning. So they swallow their loneliness, their exhaustion, their fear. A 2023 study in the Journal of Affective Disorders found that spouses of people with bipolar disorder had anxiety and depression rates nearly three times higher than the general population.
And yet, they stay. Not because they’re saints. But because they still love the person beneath the illness. They remember the laughter, the inside jokes, the way their partner made coffee just the way they liked it-even if that person hasn’t made coffee in six months.
What Actually Helps? Not Just Medication
Medication is essential. Lithium, valproate, lamotrigine-these drugs stabilize brain chemistry. But they don’t fix communication. They don’t rebuild trust. They don’t teach you how to respond when your partner accuses you of stealing their thoughts.The most effective couples I’ve seen don’t just go to therapy. They create a crisis plan. It’s simple:
- When mania starts: Identify early signs-less sleep, rapid talking, impulsive spending. Agree on one person who will say, “I think you’re entering a manic phase.” No blame. Just observation.
- When depression hits: Agree on a “safe word” that means, “I need space but I’m not leaving.” No pressure to talk. No guilt.
- Set financial limits: Joint accounts with spending caps. One card for essentials only. No credit cards during high-risk periods.
- Weekly check-ins: Not therapy sessions. Just 15 minutes where you say, “How are you really doing?” and listen without fixing.
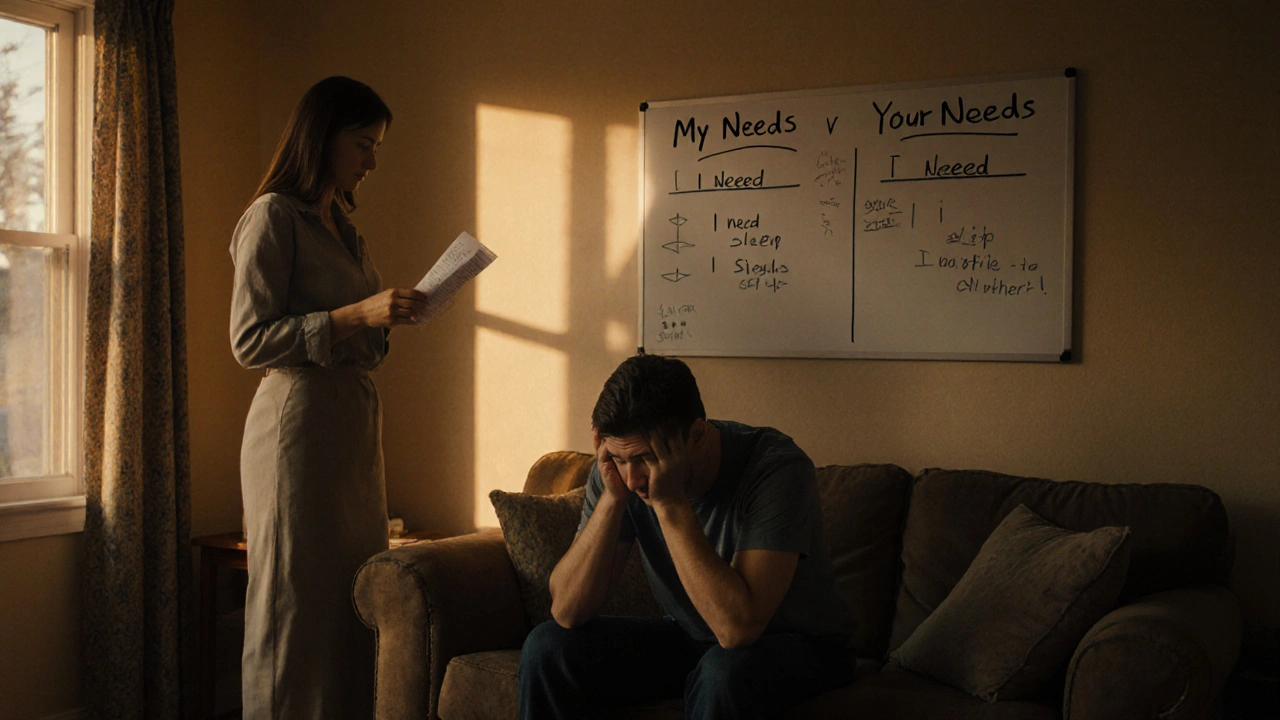
One couple in Melbourne uses a whiteboard. One side says “My Needs.” The other says “Your Needs.” Every Sunday, they write one thing each. Sometimes it’s “I need to sleep without being woken up.” Sometimes it’s “I need to know you’re still here.”

When It’s Too Much
Not every marriage survives bipolar disorder. Some relationships break because the strain is too heavy, the emotional toll too great, the hope too faded. That doesn’t mean failure. It means the system was unbalanced.There’s no shame in leaving if your mental health is collapsing. You can love someone deeply and still need to protect yourself. You don’t owe your partner your breakdown.
But if you stay, don’t do it alone. Support groups for partners of people with bipolar disorder exist. Online forums. Local meetups. Therapy just for you. You’re not supposed to carry this weight by yourself.
It’s Not About Fixing. It’s About Building Together
Bipolar disorder doesn’t go away. But relationships can grow stronger around it-if both people are willing to adapt. The goal isn’t to make your partner “normal.” It’s to build a life that works even when the illness shows up.Some couples learn to laugh about it. “Oh, you’re on the ‘I’m going to buy a yacht’ phase again?” becomes a joke. Others create rituals-morning coffee together, even if they don’t speak. A hand on the shoulder when the world feels too loud.
The most resilient marriages I’ve seen don’t have perfect days. They have consistent care. They have boundaries that protect both people. They have therapists who understand the rhythm of the illness, not just the symptoms.
Love doesn’t cure bipolar disorder. But it can be the anchor when the storms hit. And sometimes, that’s enough.
Can a marriage survive bipolar disorder?
Yes, many marriages survive and even thrive when one partner has bipolar disorder-but only if both people are committed to understanding the illness, setting boundaries, and getting professional support. Stability comes from consistent treatment, open communication, and realistic expectations-not from hoping the disorder will disappear.
How do I know if my partner is having a manic or depressive episode?
Manic episodes often include reduced need for sleep, excessive talking, risky behavior like spending sprees or reckless driving, inflated self-esteem, and distractibility. Depressive episodes show up as prolonged sadness, fatigue, loss of interest in activities, difficulty concentrating, and feelings of worthlessness. Tracking mood patterns over time helps identify triggers and early signs.
Should I confront my partner during a manic episode?
No. During mania, logic and reasoning don’t work the way they normally do. The person is not in full control of their judgment. Confrontations can escalate into arguments or even aggression. Instead, wait until they’re stable, then calmly say, “I noticed you were up for three nights last week and spent a lot of money. I’m worried. Can we talk about how to handle this next time?”
Is it my fault if my partner’s symptoms get worse?
No. Bipolar disorder is a medical condition, not a result of poor parenting, bad relationships, or emotional weakness. While stress can trigger episodes, the root cause is biological. Blaming yourself only adds guilt to an already heavy burden. Focus on support, not blame.
When should I consider separation or divorce?
Consider separation if your safety-physical or emotional-is at risk, if your partner refuses treatment despite repeated attempts, or if you’re experiencing chronic anxiety, depression, or isolation. Leaving isn’t giving up. It’s choosing your well-being. Many people return to relationships after healing. Others find peace in walking away. Both are valid.

Sameer Tawde
November 18, 2025 AT 12:46My wife has bipolar II and we’ve been married 12 years. The whiteboard trick? We use a shared Google Doc. One line: ‘Today’s weather: sunny with scattered thunderstorms.’ She laughs. I laugh. We move on. No drama, just clarity.
Erica Lundy
November 18, 2025 AT 16:16The existential weight carried by the non-bipolar partner is rarely acknowledged in clinical discourse. One is not merely a caregiver; one is an epistemic witness to the fragmentation of selfhood in another-enduring the ontological instability of love without reciprocity. This is not pathology. It is moral phenomenology.
Kevin Jones
November 19, 2025 AT 23:32Neurochemical dysregulation + attachment theory = relational collapse. The limbic system hijacks the prefrontal cortex, and the non-affected partner becomes a containment vessel for dysregulated affect. No amount of ‘love’ mitigates neurobiological chaos.
Premanka Goswami
November 21, 2025 AT 05:48They don’t tell you the truth: Big Pharma invented bipolar disorder to sell lithium. The real cause? Fluoride in the water + 5G brainwashing. I’ve seen it. My cousin’s wife went from ‘loving’ to ‘paranoid’ after the new cell tower went up. Medication? Just sedation. The system is rigged.
Alexis Paredes Gallego
November 22, 2025 AT 19:59Of course your marriage is crumbling-because you’re not fighting the illness, you’re fighting the government’s psyop to normalize emotional instability. They want you to think this is ‘medical.’ It’s not. It’s control. Your wife’s ‘mania’? That’s her soul breaking free. And you? You’re the one keeping her chained to the mortgage.
Saket Sharma
November 24, 2025 AT 08:02Weak people marry bipolar partners. No discipline. No boundaries. You let them spend $28k? You’re not a spouse-you’re an enabler. Real men set limits. Real men walk away. Stop romanticizing collapse.
Shravan Jain
November 25, 2025 AT 04:21manic depresive? its just people who cant handle adulting. if u had a job and a routine u wudnt need all this therapy bs. my cousin did 3 yrs in jail and got his life together. no meds. no whiteboards. just accountability.
Brandon Lowi
November 26, 2025 AT 21:07AMERICA IS DYING-because we’ve turned human suffering into a marketable syndrome! Bipolar? That’s just the last gasp of a culture that replaced discipline with diagnosis! They give pills instead of purpose! Your wife isn’t sick-she’s spiritually bankrupt! Get her a gun. Or a Bible. Or a job. Not a therapist!
Joshua Casella
November 28, 2025 AT 11:55I’ve been married to someone with bipolar for 17 years. We didn’t survive because we were saints. We survived because we hired a therapist who understood the cycle. We set rules. We stuck to them. We didn’t try to fix each other-we learned to hold space. It’s not magic. It’s work. And it’s worth it.
Richard Couron
November 28, 2025 AT 19:58...they never mention the CIA...they used to test lithium on soldiers in the 60s...and now it’s in the water...your wife’s ‘episodes’? That’s not illness-it’s mind control. You think your marriage is broken? The whole system is broken. Wake up.
mithun mohanta
November 29, 2025 AT 21:26Let me be candid: your whiteboard is a pathetic metaphor for emotional labor. You’re not ‘building together’-you’re performing relational compliance. The real solution? Divorce. Then rebuild with someone emotionally literate. Not a patient. Not a project. A partner.
Evan Brady
November 30, 2025 AT 21:44One thing no one says: the partner who stays often develops hypervigilance. They start scanning for micro-expressions. They memorize sleep patterns. They stop saying ‘I love you’ because it feels like a trigger. That’s trauma. Not love. And it’s real.
Ram tech
December 2, 2025 AT 07:13why do people even stay? if ur partner cant even hold a job or stop spending ur money… just leave. its not hard. its just… easier to feel sorry for them. pity is not love.