How to Read Medication Guides for Risk and Monitoring Advice
 Nov, 12 2025
Nov, 12 2025
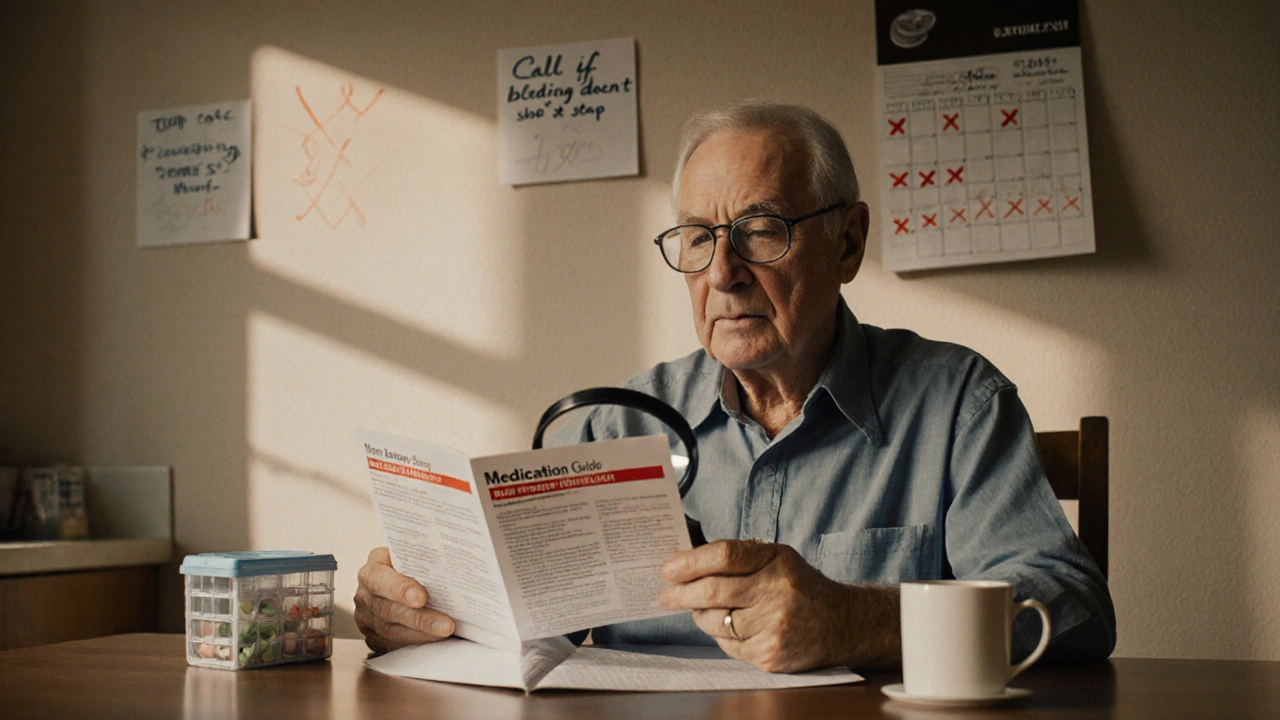
When you pick up a new prescription, you’re handed a small paper - the Medication Guide. It looks like just another form to sign, another thing to shove in your bag. But this piece of paper could literally save your life. The FDA requires these guides for drugs with serious, preventable risks. And yet, most people never read them. Not because they don’t care, but because they don’t know how to read them.
What Makes a Medication Guide Different?
Not every drug comes with a Medication Guide. Only those with risks so serious they can be avoided if you know what to watch for. That’s why the FDA mandates them. These aren’t the same as the small print inside the bottle or the instructions your pharmacist gives you. Medication Guides are legally required to be written in plain language - no medical jargon, no tiny fonts. They’re designed for a 6th to 8th grade reading level. That means you don’t need a science degree to understand them.There are about 150 of these guides in use right now. They cover everything from blood thinners like warfarin to antidepressants, immunosuppressants like Humira, and even newer drugs like deucravacitinib for psoriasis. Each one is updated within 30 days if new safety info comes out. So if you’ve had the same medication for years, check if the guide changed.
The 4 Sections That Matter Most
You don’t need to read the whole thing. There are four sections that hold all the life-saving info. Find these first:- What is the most important information I should know about [drug name]? This is where the FDA puts the big red flags. It’s not vague. It says things like: “Can cause serious liver damage” or “May lead to a dangerous drop in white blood cells.” This is the section that tells you if the drug could hurt you - and how.
- What are the possible or reasonably likely serious side effects? This isn’t a list of “might feel a little dizzy.” It’s specific: “Get your blood tested every 3 months to check for changes in blood cell counts.” It tells you exactly what to monitor and how often.
- What should I tell my healthcare provider before taking [drug name]? This tells you what conditions or medications could make this drug dangerous for you. If you have liver disease, kidney problems, or are on another drug that interacts with it - this section will say so.
- How should I take [drug name]? This is where the monitoring schedule lives. It doesn’t just say “take once daily.” It says: “Your doctor will test your blood before you start and every month after.” It might warn you not to drink alcohol, avoid the sun, or never stop suddenly.
For example, the warfarin (Coumadin) guide says: “If your dose is changed, your INR should be checked more often.” It lists exact symptoms that mean trouble: “Unusual bruising or bleeding that lasts a long time.” That’s not something you can guess. That’s something you need to know before it’s too late.
How to Spot the Red Flags
Pharmacists and patient safety experts have identified seven phrases that should make you stop and pay attention. If you see any of these, highlight them:- “Get blood tests regularly”
- “Call your doctor immediately if…”
- “Do not stop taking without talking to your doctor”
- “Avoid sunlight exposure”
- “Do not drink alcohol”
- “May impair driving ability”
- “Keep all scheduled appointments”
These aren’t suggestions. They’re safety rules. If your guide says “get your blood tested monthly,” that means every 30 days - not “when you feel off.” A 2022 survey found that 28% of patients thought “monitor monthly” meant “only if something feels wrong.” That’s a deadly misunderstanding.

Use the Traffic Light System
One of the most effective tools patients use is the “traffic light” method. It’s simple:- Green - Normal symptoms. Mild nausea, fatigue, or headache that goes away after a few days.
- Yellow - Warning signs. These need monitoring. For example: “Your INR is a little high,” or “You’re feeling more anxious than usual.” Call your doctor within 24 hours.
- Red - Emergency. These mean go to the ER or call 911. Like: “You’re bleeding from your gums and can’t stop,” or “You suddenly can’t breathe.”
Patients who used this system had 55% better adherence to monitoring schedules. It turns confusing text into clear action. You don’t have to remember every word. Just remember: green = okay, yellow = call, red = go now.
How to Read It Without Getting Overwhelmed
Most people give up because the guide looks like a textbook. But you don’t need to read it all at once. Use the FDA’s 3-2-1 method:- 3 minutes - Read it before you take your first dose. Focus only on the four sections above.
- 2 minutes - Before each refill, flip through it again. Has anything changed? Did they add a new warning?
- 1 minute - Every time you take your pill, ask: “Is today the day I need to get tested?”
Harvard Medical School found that guides using numbers - like “25% of patients experience dizziness” - are 47% more understandable than vague ones like “may cause dizziness.” So if your guide says “About 1 in 200 people taking clozapine may develop agranulocytosis,” that’s not scare tactics. It’s real data. And you need to know it.

What to Do If You Don’t Get the Guide
The law says you must get a Medication Guide every time you pick up the prescription. But a 2022 audit found 41% of independent pharmacies didn’t always give them out. If you don’t get one, ask for it. If they say they don’t have it, call your doctor or go to DailyMed.gov - the NIH’s official site for all FDA-approved guides. You can download, print, and bring it to your next appointment.People who recorded their monitoring schedule in a journal had 68% fewer bad reactions. Write down: “Blood test every 3 months - next one due on June 15.” Put it on your fridge. Set a phone reminder. Make it part of your routine.
What’s Changing in 2025?
The system is getting better. By 2025, all drugs with Risk Evaluation and Mitigation Strategies (REMS) will need a Medication Guide. That’s 127 drugs - up from 42. The FDA is testing QR codes on pill bottles that link directly to the latest guide. Pfizer is piloting AI guides that personalize risk info based on your age, other meds, and health history. Early results show patients understand their risks 63% better.But here’s the catch: 40% of U.S. adults struggle with health literacy. No matter how clear the guide is, if you can’t read it, it won’t help. That’s why your pharmacist or doctor should walk you through it. Don’t be shy. Say: “Can you help me understand the red flags in this guide?”
Why This Matters More Than You Think
The FDA studied 500 patients. Those who followed the monitoring advice in their Medication Guide had 32% fewer serious side effects. That’s not a small number. That’s thousands of hospital visits avoided. That’s lives saved.It’s not about being perfect. It’s about being aware. You don’t have to memorize every word. But you do need to know: What’s the worst thing that could happen? What test do I need? When? And what symptom means I should run to the ER?
Next time you get a new prescription, don’t just sign the form. Take two minutes. Find those four sections. Highlight the red flags. Set a reminder. That’s all it takes. Because when it comes to your health, the most dangerous thing isn’t the drug. It’s not knowing what to watch for.
Are Medication Guides the same as the instructions that come with my pill bottle?
No. The small leaflet inside the bottle is usually a general instructions sheet. Medication Guides are separate, FDA-mandated documents that focus only on serious, preventable risks. They’re written in plain language and must be given to you every time you fill a prescription for certain high-risk drugs.
What if I don’t understand the language in the guide?
You’re not alone. Many guides are written at a 6th-8th grade level, but if you still struggle, ask your pharmacist or doctor to explain it. Most pharmacies offer free counseling. You can also call the drug manufacturer’s patient support line - they’re required to help. And you can always download the guide from DailyMed.gov and bring it to your appointment for review.
How often are Medication Guides updated?
Manufacturers must update guides within 30 days of new safety information being approved by the FDA. In 2022, 92% of guides were updated - up from 85% in 2021. Always check the date on the guide. If you’ve been taking the same medication for a while, ask if there’s a newer version.
Can I rely on my doctor to explain all the risks?
Doctors are busy, and they can’t cover every risk in a 10-minute visit. Medication Guides exist because not all risks can be communicated quickly. They’re your backup. Read them yourself. Then bring your questions to your doctor. It’s your right to understand your treatment - and the guide is your best tool for that.
What if I miss a blood test or monitoring appointment?
Missing a test doesn’t mean you’re in immediate danger - but it increases your risk. Many serious side effects only show up through blood tests before you feel symptoms. If you miss one, call your doctor right away. Don’t wait for your next appointment. Some drugs, like clozapine or warfarin, require strict timing - missing a test can lead to life-threatening complications.
Do all prescription drugs have Medication Guides?
No. Only drugs with serious, preventable risks require them. That’s about 150 medications out of thousands. Common ones include blood thinners, antidepressants, immunosuppressants, and certain cancer drugs. If you’re unsure, ask your pharmacist or check DailyMed.gov.
Can I get a digital copy of my Medication Guide?
Yes. The NIH’s DailyMed website has every FDA-approved Medication Guide available for free download. You can search by drug name or brand. Many pharmacies also email or text digital copies if you ask. Keep a copy on your phone - it’s easier to check than carrying paper.

Esperanza Decor
November 14, 2025 AT 04:55I used to ignore these guides until my mom had a near-fatal reaction to warfarin because she didn't know to check her INR every 3 weeks. Now I print every one out and stick it on the fridge next to the milk. It’s not glamorous, but it’s saved us more than once.
Pro tip: If the guide says ‘call your doctor immediately if,’ write that phrase in big letters on a sticky note and put it on your bathroom mirror. You’ll see it every morning.
Also, don’t wait for your refill to check the date. I once missed a warning about liver toxicity because I assumed it hadn’t changed since 2020. It had. Updated in January. I didn’t look.
It’s not paranoia. It’s responsibility.
Thanks for this. I’m sharing it with my book club.
Deepa Lakshminarasimhan
November 14, 2025 AT 21:17They’re not just guides. They’re tracking devices. The government forces these because they know people will die if we’re left to guess. Same way they force seatbelts. Same way they ban certain chemicals. This is control dressed up as care.
Who decides what’s a ‘serious’ risk? Pharma lobbyists? The FDA gets funding from the same companies that make these drugs. Coincidence? I don’t think so.
They give you the guide so you feel like you’re in control. But you’re still just a number in their algorithm. Read it all you want - they’ll still profit whether you live or die.
Erica Cruz
November 15, 2025 AT 00:52Let’s be real - this is just corporate theater. The FDA doesn’t care if you live or die. They care about liability. That’s why these guides exist: so when someone dies from a side effect, they can say ‘We warned them.’
And don’t get me started on the ‘6th grade reading level’ nonsense. That’s not accessibility - it’s condescension. If you can’t read a medical document, maybe you shouldn’t be taking prescription drugs at all.
Also, QR codes? AI guides? Please. This is just pharma’s next marketing gimmick to make you feel like they’re ‘innovating’ while they jack up prices 400%.
Johnson Abraham
November 15, 2025 AT 06:27lol i read one of these once and thought it was a joke. like ‘do not drink alcohol’?? who even drinks with meds??
then i got drunk after taking my antidepressant and woke up in the hospital. yeah. that happened.
now i read em. kinda. mostly i just screenshot the red flags and send them to my bro who’s a nurse.
also why do they always say ‘call your doc’ like that’s gonna fix anything? doc’s busy. nurse’s the one who actually knows stuff.
tl;dr: read the damn thing. i’m not your mom but i’m glad i did.
Shante Ajadeen
November 16, 2025 AT 07:20This is the kind of post I wish I’d seen five years ago. I used to panic every time I got a new script - too overwhelmed to read anything. Now I use the traffic light system and it’s changed everything.
Green: I take my pill and go about my day.
Yellow: I jot it down and call my pharmacist the next day - they’re always happy to help.
Red: I go to urgent care. No hesitation.
My doctor says I’m the most prepared patient he’s ever had. I just followed the guide. No magic. Just clarity.
Thank you for writing this. I’m printing copies for my mom and my sister. They both have chronic conditions. They deserve this info too.
dace yates
November 16, 2025 AT 13:37Do the updated guides include info on drug interactions with over-the-counter supplements? I take turmeric and magnesium daily and I’ve never seen those mentioned. Should I assume they’re safe or is that a blind spot?
Danae Miley
November 17, 2025 AT 11:59You’re missing a critical point: Medication Guides are not legally required to be distributed in non-English languages, even though 22% of U.S. households speak a language other than English at home. The FDA mandates plain language - but not multilingual access. This is systemic health inequity disguised as patient education.
And yet, you’re praising the 6th-grade reading level? That’s not empowerment - it’s linguistic gatekeeping. If your guide is only in English, it’s useless to 50 million Americans. This isn’t progress. It’s exclusion dressed as accessibility.
Charles Lewis
November 19, 2025 AT 11:52While the structure and intent of the Medication Guide are commendable, I would argue that the true barrier to adherence lies not in comprehension but in systemic fragmentation. The patient is expected to reconcile information from the guide, the pharmacist’s verbal instructions, the physician’s abbreviated counseling, the electronic health record’s medication list, and the pharmacy’s digital portal - all of which may contain conflicting or outdated data.
Furthermore, the reliance on self-monitoring without integrated digital alerts or automated lab result notifications creates a cognitive burden disproportionate to the patient’s capacity, particularly among elderly, neurodivergent, or low-literacy populations.
True innovation lies not in QR codes or AI summaries, but in interoperable systems that push critical alerts directly to the patient’s phone or caregiver’s device when a lab window is missed or a contraindication arises. The guide is a stopgap. We need infrastructure.
Renee Ruth
November 20, 2025 AT 05:14I read the guide for my antidepressant and found out it could cause suicidal thoughts in people under 25. I’m 23.
I didn’t know.
I didn’t know until I read it myself.
My doctor never mentioned it. My pharmacist just handed me the bottle.
Two weeks later, I tried to kill myself.
I didn’t die.
But I wish I’d known before I swallowed that first pill.
This guide saved my life - but only because I was desperate enough to read it.
Why is it on us to save ourselves?
Why isn’t someone telling us this before we take it?
Samantha Wade
November 21, 2025 AT 16:30This is exactly the kind of public health education we need - clear, actionable, and rooted in evidence. I’ve trained dozens of patients using the traffic light system, and the results are undeniable: fewer ER visits, better adherence, and more empowered individuals.
But we must go further. Hospitals and pharmacies must be mandated to provide in-person, 5-minute guided walkthroughs of the Medication Guide upon dispensing - not just handing out paper. Insurance companies should reimburse for this. It’s preventive care at its most cost-effective.
And to those who say, ‘It’s the patient’s responsibility’ - no. It’s ours. As clinicians, as pharmacists, as community members. We are the safety net. Let’s stop pretending the guide alone is enough.
Thank you for making this accessible. Now let’s make it universal.
Elizabeth Buján
November 23, 2025 AT 07:06I used to think reading these guides was for people who overthink everything. Like, ‘I’m fine, why stress?’
Then my best friend had a seizure because she missed the ‘avoid sunlight’ warning on her psoriasis drug. She was outside for five minutes. Five minutes.
Now I carry a copy of every guide I get on my phone. I read it before I take the pill. I talk to my mom about it. I even made a little checklist on my Notes app.
It’s not about being scared. It’s about being awake.
These papers? They’re not paperwork. They’re lifelines.
And if you’re not reading them? You’re not just ignoring a rule.
You’re ignoring your own survival.
So do it. Just once. For you.