Lquin (Levofloxacin) vs. Other Antibiotics: A Practical Comparison
 Oct, 5 2025
Oct, 5 2025
Antibiotic Selection Guide: Lquin vs. Alternatives
Lquin (Levofloxacin)
Third-generation fluoroquinolone, excellent lung penetration, once-daily dosing.
- Primary use: Pneumonia, sinusitis, UTI
- Side effects: Tendon rupture, QT-prolongation
- Cost: ~AU$30-45 for 10-day course
Ciprofloxacin
Second-generation fluoroquinolone, strong against gram-negative bacteria.
- Primary use: UTI, skin infections
- Side effects: Tendon issues, CNS effects
- Cost: ~AU$20-35 for 10-day course
Moxifloxacin
Newer fluoroquinolone with strong anaerobic activity.
- Primary use: Intra-abdominal infections
- Side effects: QT-prolongation, hepatic issues
- Cost: ~AU$45-60 for 10-day course
Doxycycline
Tetracycline antibiotic, good for atypical pneumonia and Lyme disease.
- Primary use: Atypical pneumonia, Lyme disease
- Side effects: Photosensitivity, esophagitis
- Cost: ~AU$10-20 for 10-day course
Amoxicillin
Beta-lactam penicillin, broad-spectrum coverage for upper respiratory infections.
- Primary use: Ear, nose, throat infections
- Side effects: Allergic rash, GI upset
- Cost: ~AU$8-15 for 10-day course
Clarithromycin
Macrolide antibiotic, effective for atypical respiratory infections.
- Primary use: Atypical pneumonia, H. pylori
- Side effects: GI upset, hepatic enzyme rise
- Cost: ~AU$15-25 for 10-day course
Decision Matrix
Use Lquin or Moxifloxacin for lung-focused infections where fluoroquinolones are safe.
Use Doxycycline or Amoxicillin if there's a high risk of tendon injury or QT-prolongation.
Use Clarithromycin for atypical pathogens when macrolides are appropriate.
Use Ciprofloxacin or Beta-Lactams for resistant gram-negative UTIs.
Safety Tips
- Avoid vigorous exercise during treatment
- Screen for tendon disorders and steroid use
- Monitor electrolytes if on diuretics
- Warn about vivid dreams or confusion in elderly
Key Takeaway
Match antibiotic choice to the suspected pathogen, patient factors, and local resistance patterns. Consider cost, dosing convenience, and drug interactions when making clinical decisions.
Quick Summary / Key Takeaways
- Lquin is the brand name for Levofloxacin, a widely used fluoroquinolone.
- Key alternatives include ciprofloxacin, moxifloxacin, doxycycline, amoxicillin and clarithromycin.
- Levofloxacin offers once‑daily dosing and good lung penetration but carries a higher risk of tendon issues.
- Choosing an alternative depends on infection site, resistance patterns, patient age and side‑effect tolerance.
- Cost, drug interactions and local formulary restrictions often tip the balance in real‑world prescribing.
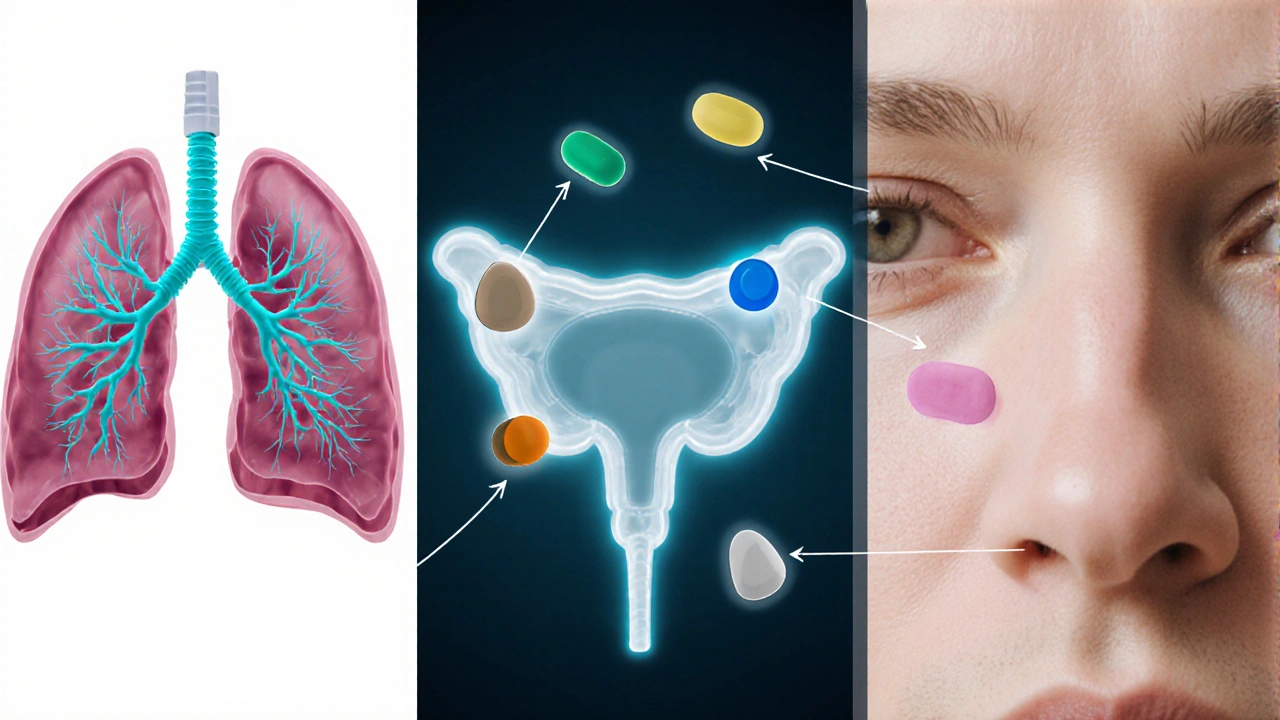
When doctors need to treat a bacterial infection, they often reach for Lquin - the commercial name for a fluoroquinolone antibiotic called levofloxacin. While Lquin works well for many respiratory and urinary infections, patients and clinicians frequently ask whether another drug might be safer, cheaper, or more appropriate for a specific bug.
This guide walks through the most common alternatives, compares how they stack up on effectiveness, safety, dosing convenience and price, and gives you a clear decision‑making framework.
What is Lquin (Levofloxacin)?
Levofloxacin is a third‑generation fluoroquinolone that blocks bacterial DNA gyrase and topoisomerase IV, preventing DNA replication. Approved in the early 2000s, it quickly became a go‑to for community‑acquired pneumonia, acute sinusitis, and uncomplicated urinary tract infections. Typical adult dosing is 500mg once daily for 5‑10days, though a 750mg dose is used for severe pneumonia.
Key attributes of Lquin include:
- Broad gram‑negative and gram‑positive coverage.
- Excellent lung and prostate tissue penetration.
- Generally well tolerated, but may cause tendon rupture, QT‑prolongation, and CNS effects.
Common Alternatives to Levofloxacin
Below are the five most frequently prescribed rivals, each with its own niche.
Ciprofloxacin is a second‑generation fluoroquinolone that excels against gram‑negative organisms like Escherichia coli and Pseudomonas aeruginosa.
Moxifloxacin is a newer fluoroquinolone with stronger anaerobic activity, making it useful for intra‑abdominal infections.
Doxycycline belongs to the tetracycline class and is favored for atypical pneumonia, Lyme disease and acne.
Amoxicillin is a beta‑lactam penicillin that covers many gram‑positive and some gram‑negative bacteria, especially in ear, nose, throat infections.
Clarithromycin is a macrolide antibiotic often used for atypical respiratory infections and Helicobacter pylori eradication.
Comparison Table: Efficacy, Safety & Practicality
| Attribute | Lquin (Levofloxacin) | Ciprofloxacin | Moxifloxacin | Doxycycline | Amoxicillin | Clarithromycin |
|---|---|---|---|---|---|---|
| Primary Spectrum | Gram‑neg + gram‑pos, atypicals | Gram‑neg (incl. Pseudomonas) | Gram‑neg + anaerobes | Atypicals, intracellular | Gram‑pos, some gram‑neg | Atypicals, Mycoplasma |
| Dosing Frequency | Once daily | Twice daily | Once daily | Twice daily | Three times daily (or BID) | Twice daily |
| Typical Course Length | 5‑10days | 7‑14days | 5‑10days | 7‑14days | 5‑10days | 7‑14days |
| Key Side‑effects | Tendon rupture, QT‑prolongation | Tendon issues, CNS | QT‑prolongation, hepatic | Photosensitivity, esophagitis | Allergic rash, GI upset | GI upset, hepatic enzyme rise |
| Resistance Concerns | Increasing fluoroquinolone resistance | High for E. coli | Low but emerging | Low, but tetracycline resistance noted | Beta‑lactamase producing strains | Macrolide‑resistant Streptococcus pneumoniae |
| Cost (AU$) - 10‑day course | ≈$30‑45 | ≈$20‑35 | ≈$45‑60 | ≈$10‑20 | ≈$8‑15 | ≈$15‑25 |
How to Choose the Right Antibiotic
Think of antibiotic selection as a balance sheet. List the infection’s likely pathogen, the drug’s spectrum, patient‑specific factors, and the practicalities of dosing and cost.
- Identify the likely bug. Community‑acquired pneumonia often involves S. pneumoniae (gram‑pos) plus atypicals. For urinary tract infections, E. coli dominates.
- Check local resistance data. In Brisbane, fluoroquinolone resistance in E. coli is climbing above 20%.
- If resistance is high, consider amoxicillin‑clavulanate or doxycycline.
- Assess patient risk factors. Elderly patients, those on steroids, or with a history of tendon problems should avoid Lquin and other fluoroquinolones.
- For a 70‑year‑old with osteoarthritis, doxycycline or amoxicillin may be safer.
- Factor in drug interactions. Lquin can increase serum levels of warfarin and theophylline. Clarithromycin interacts with statins.
- Consider convenience. Once‑daily dosing (Lquin, moxifloxacin) improves adherence compared with thrice‑daily regimens.
- Look at cost and formulary. In many Australian private scripts, amoxicillin is the cheapest, while fluoroquinolones may require prior‑authorisation.
Summarise the above in a quick decision matrix:
- If the infection is lung‑focused and patient tolerates fluoroquinolones → Lquin or moxifloxacin.
- If there’s a high risk of tendon injury or QT‑prolongation → Doxycycline or amoxicillin.
- If atypical pathogens dominate and a macrolide is appropriate → Clarithromycin.
- If gram‑negative urinary infection with known fluoroquinolone resistance → Ciprofloxacin (if susceptible) or a beta‑lactam with a beta‑lactamase inhibitor.
Safety Tips When Using Fluoroquinolones
Fluoroquinolones, including Lquin, have received FDA boxed warnings for tendon rupture, peripheral neuropathy, and central nervous system effects. Here’s how to minimise risk:
- Advise patients to avoid vigorous exercise for a week after starting therapy.
- Screen for a history of tendon disorders, steroid use, or elderly age.
- Monitor electrolytes if the patient is on diuretics, as low potassium can worsen QT‑prolongation.
- Warn about possible vivid dreams or confusion, especially in older adults.

When Lquin is the Clear Choice
Despite its cautions, Lquin shines in scenarios where other agents fall short:
- Severe community‑acquired pneumonia needing high lung concentrations.
- Complicated urinary tract infections caused by resistant gram‑negative organisms where beta‑lactams fail.
- Patients who need a once‑daily regimen due to adherence concerns.
In such cases, the benefits outweigh the potential drawbacks, especially when duration is limited to 5‑7days.
Key Takeaways for Clinicians and Patients
- Match spectrum to suspected pathogen before defaulting to Lquin.
- Check local antibiograms; rising fluoroquinolone resistance can make alternatives more effective.
- Consider patient age, comorbidities, and drug‑interaction profile.
- Use the comparison table to discuss cost and dosing convenience with the patient.
- Reserve Lquin for infections where its pharmacokinetic advantages are truly needed.
Frequently Asked Questions
Can I take Lquin if I’m pregnant?
Fluoroquinolones are generally contraindicated in pregnancy because they can affect fetal cartilage development. Safer alternatives like amoxicillin or cefalexin are preferred unless no other option exists.
How does Lquin compare to moxifloxacin for pneumonia?
Both are once‑daily fluoroquinolones, but moxifloxacin has stronger activity against anaerobes and atypicals. Lquin offers slightly broader gram‑negative coverage. Clinical guidelines often list moxifloxacin as the first‑line fluoroquinolone for severe pneumonia because of its better tissue penetration.
What should I do if I experience tendon pain while on Lquin?
Stop the medication immediately and contact your doctor. Tendon pain can be an early sign of rupture. Your physician will likely switch you to a non‑fluoroquinolone antibiotic and may order imaging if the pain is severe.
Is a 5‑day course of Lquin enough for a urinary tract infection?
For uncomplicated cystitis caused by susceptible E. coli, a 5‑day course of 500mg once daily is usually sufficient. Complex infections or resistant strains may require longer treatment or a different agent.
Why is Lquin more expensive than amoxicillin?
Levofloxacin is a newer, patented molecule with a broader spectrum, leading to higher manufacturing costs and a more complex regulatory pathway. Amoxicillin is an older, off‑patent drug produced in large volumes, which drives its low price.

Aaron Perez
October 5, 2025 AT 13:08In the grand theater of antimicrobial selection, one must first contemplate the ontology of the pathogen, the epistemology of the drug’s mechanism, and the teleology of patient outcomes; only then can one discern the subtle hierarchies that render Lquin both a boon and a bane, a paradoxical talisman in the physician’s armamentarium, a double‑edged sword that slices through bacterial DNA yet threatens our very tendons, a reminder that every therapeutic triumph is shadowed by a latent risk, a truth that the modern practitioner must internalize, a dictum that the naïve prescriber often overlooks.
William Mack
October 17, 2025 AT 21:42Great breakdown! The table makes it super easy to pick the right drug for the right infection. 👍
Evan Riley
October 30, 2025 AT 05:16Look, while everyone is busy praising fluoroquinolones, what they don’t tell you is how Big Pharma pushes Lquin onto unsuspecting patients under the guise of convenience. The regulatory agencies are complicit, approving it faster than they should, while the data on tendon rupture is being buried. Every prescription is a covert operation to keep the drug on the market, and the very guidelines you quote are drafted by consultants with stakes in the sales figures. If you dig deeper, you’ll find that the “once‑daily dosing” claim is a marketing ploy to hide the fact that compliance is still low because of side‑effects that are systematically down‑played. The truth is, Lquin is a perfect storm: powerful enough to wipe out bugs, dangerous enough to cause lasting harm, and profitable enough to keep the cycle going. So before you hand out Lquin, remember that the unseen hand of the industry is pulling the strings, and the patient pays the price.
Nicole Povelikin
November 11, 2025 AT 13:50Sure, but why not just use amoxicillin?
Michelle Weaver
November 23, 2025 AT 22:25Let’s take a step back and appreciate the nuance in antibiotic stewardship. 💡 The decision matrix presented here does more than just list prices; it integrates pharmacokinetics, tissue penetration, and patient‑specific risk factors into a cohesive framework. For instance, Lquin’s superior lung concentration makes it a compelling choice for severe community‑acquired pneumonia, especially when the pathogen profile suggests atypical organisms that might evade beta‑lactams. On the other hand, the risk of tendon rupture, QT‑prolongation, and CNS effects cannot be brushed aside, particularly in the elderly or those on concurrent steroids. Cost considerations are also pivotal-while Lquin sits at $30‑45 for a 10‑day course in Australia, a course of doxycycline can be obtained for as little as $10‑20, offering a budget‑friendly alternative for atypical coverage. Moreover, the local antibiogram data you referenced highlights a rising fluoroquinolone resistance in E. coli, nudging clinicians toward agents like amoxicillin‑clavulanate or a tailored beta‑lactamase inhibitor regimen. Another layer is drug‑drug interactions: Lquin can elevate warfarin levels, a nuance that matters in patients with atrial fibrillation. In contrast, macrolides such as clarithromycin carry their own interaction profile, especially with statins, but they shine against Mycoplasma and Chlamydophila. The safety tips are spot‑on-advise patients to avoid vigorous exercise and monitor electrolytes if they’re on diuretics, thereby mitigating QT risks. Finally, the patient‑centered approach-discussing dosing convenience, potential side‑effects, and cost-empowers shared decision‑making, which improves adherence and outcomes. In short, this guide equips clinicians with a balanced, evidence‑based tool to navigate the complex terrain of antimicrobial selection. 🌟
John Keough
December 6, 2025 AT 06:59I agree with the thoroughness of the guide; the mix of efficacy data and practical tips really helps when choosing a regimen for a busy clinic. It’s a solid reference.
Graham Smith
December 18, 2025 AT 15:33There’s a typo in “fluoroquinolones” – it’s written as “fluroquinolones”. Also, “beta‑lactams” should be hyphenated consistently.
Jeremiah Morgan
December 31, 2025 AT 00:07Excellent summary! Your emphasis on patient‑specific factors really highlights the art of medicine, and the clear tables make it all the more accessible.
nina greer
January 12, 2026 AT 08:42While the guide is thorough, the overly simplistic cost comparison undermines its academic rigor.
Montague Tilmen
January 24, 2026 AT 17:16Our healthcare system should prioritize American‑made antibiotics like Lquin over foreign imports; we must keep the industry strong.
Clarise Wheller
February 6, 2026 AT 01:50Let’s remember that collaboration across specialties, rather than nationalism, yields the best patient outcomes.
Riley Fox
February 18, 2026 AT 10:25Ah! The elegance of a well‑crafted comparison-one observes, contemplates, and then critiques: the over‑use of fluoro‑quinolones, the under‑appreciated value of beta‑lactams; indeed, the balance is fragile; however, the author seems to have omitted mention of emerging resistance trends in Acinetobacter, which is a glaring oversight, wouldn’t you agree? 🤔