Steroid‑Induced Cataract: Symptoms, Risks & Treatment
 Oct, 25 2025
Oct, 25 2025
Steroid Cataract Risk Calculator
Understand Your Risk
This calculator estimates your risk of developing steroid-induced cataracts based on usage patterns and health factors. The data is based on clinical studies referenced in the article.
Risk assessment will appear here
Your risk level will be displayed after calculation
Key Takeaways
- Steroid‑induced cataracts are usually posterior subcapsular cataracts that can develop within weeks to months of steroid use.
- Typical vision changes include blurry near vision, glare, halo effects around lights, and faded colors.
- Higher daily doses, longer treatment duration, and topical steroids raise the risk dramatically.
- Early detection through regular eye exams can delay surgery and preserve visual quality.
- When surgery is needed, cataract removal with an intraocular lens restores vision, but ongoing steroid therapy may require extra monitoring.
When doctors prescribe corticosteroids for conditions such as asthma, rheumatoid arthritis, or uveitis, they focus on quelling inflammation. What many patients don’t realise is that those same steroids can cloud the eye’s natural lens-creating a steroid induced cataract. This article breaks down how the condition forms, what visual clues to look for, which patients are most vulnerable, and how surgeons fix the problem while keeping the underlying disease under control.
Steroid‑Induced Cataract is a type of posterior subcapsular cataract (PSC) that arises directly from exposure to corticosteroids. Unlike age‑related cataracts that develop over years, PSCs can appear after just a few weeks of high‑dose steroid therapy.How Steroids Turn the Lens Opaque
The lens is a clear, protein‑rich structure that stays transparent because its proteins stay perfectly ordered. Corticosteroids interfere with that order in two main ways:
- Chemical binding: The C‑20 ketone group of steroids forms Schiff‑base intermediates with lens proteins, followed by a Heyns rearrangement that creates stable, non‑breakable adducts. These adducts have only been found in steroid‑related cataracts.
- Oxidative stress: Steroids suppress the eye’s natural antioxidant enzymes, tipping the balance toward free‑radical damage. The result is microscopic protein clumps that scatter incoming light, especially in the posterior subcapsular region where light first focuses.
Because the lens lacks blood vessels, it can’t easily replace damaged proteins. Over time the clumps become visible as tiny opacities that grow into full‑blown PSCs.
Who Is Most at Risk?
Not every steroid user will develop a cataract, but certain patterns dramatically raise the odds:
- Dosage: Daily exposure to more than 2,000 mg of beclomethasone (or an equivalent dose of any potent steroid) triples the likelihood of PSC formation.
- Duration: Four months of continuous use is enough to trigger lens changes; some patients notice early opacities after just 2-4 weeks.
- Route: Topical ocular steroids carry a 3.2‑fold higher relative risk than systemic steroids, according to a 2024 Al Ahsa City study.
- Age & pre‑existing disease: Children on long‑term steroids, diabetics, and patients with uveitis face compounded risk because their lenses already battle oxidative stress.
In a 2023 review of 8.9 % of long‑term steroid users, the majority of cases were linked to eye drops used for chronic inflammation.
What Vision Changes Signal a Problem?
Because PSCs sit directly in the path of incoming light, even tiny clouds disrupt vision. The most common complaints, compiled from Healthline’s 2023 patient survey, include:
- Blurry near vision (92 % of patients)
- Faded or washed‑out colors (78 %)
- Glare and halo effects around streetlights or headlights (83 %)
- Double vision, especially in low‑light environments (45 %)
- Reduced peripheral vision (67 %)
- Night‑time reading difficulty (76 %)
These symptoms often appear faster than with age‑related cataracts, prompting many patients to seek surgery within a year of onset.
Spotting the Early Signs - The Role of the Eye Exam
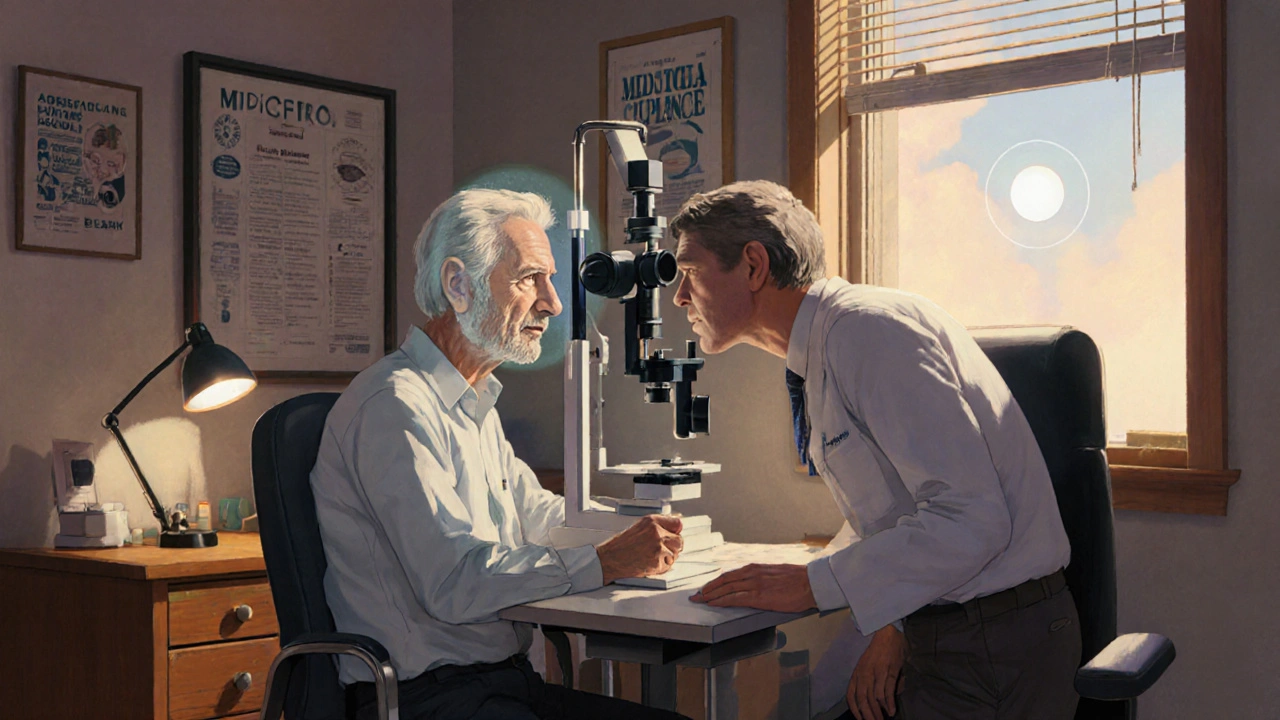
Routine monitoring is the most effective defense. The Mayo Clinic recommends a baseline slit‑lamp biomicroscopy exam before initiating any steroid course longer than two weeks, followed by checks every three to four months for high‑risk individuals.
During a slit‑lamp exam, ophthalmologists look for:
- Fine, grayish opacities just behind the posterior capsule.
- Increased light scatter on retro‑illumination photographs.
- Any change in intra‑ocular pressure that could hint at steroid‑induced glaucoma.
Early detection often means the cataract is still small enough to monitor without immediate surgery, especially if the steroid regimen can be tapered.
When Surgery Becomes Inevitable
Once visual impairment interferes with daily tasks-reading, driving at night, or recognizing faces-cataract extraction is the definitive solution. The procedure, standardised across the globe, involves two steps:
- Phacoemulsification breaks up the cloudy lens with ultrasonic energy.
- An artificial intraocular lens (IOL) is implanted, restoring a clear optical pathway.
In the context of steroid‑induced PSCs, surgery outcomes are excellent: the London Cataract Centre reports a 92 % rate of significant visual improvement. However, patients who must stay on steroids after surgery need tighter postoperative follow‑up because ongoing inflammation can affect IOL positioning or cause posterior capsular opacification.
Cataract Surgery removes the clouded natural lens and replaces it with a clear artificial intraocular lens, allowing light to focus properly on the retina.Managing Steroid Therapy Around Surgery
Ideally, doctors try to lower the steroid dose before the operation. When reduction isn’t possible-say, for severe uveitis-surgeons may add peri‑operative anti‑inflammatory drops (e.g., prednisolone acetate) to protect the eye while the IOL heals.
Patients should never stop steroids abruptly without a physician’s guidance, as a flare‑up of the underlying disease could jeopardise vision even more than the cataract.
Prevention Strategies for High‑Risk Patients
Aside from regular eye checks, several proactive steps can blunt the cataract‑forming process:
- Use the lowest effective steroid dose: Follow the principle of “as low as reasonably achievable” (ALARA) championed by the American Academy of Ophthalmology.
- Consider steroid‑sparing alternatives: For some conditions, non‑steroidal anti‑inflammatories or biologic agents can reduce exposure.
- Antioxidant supplementation: Early studies suggest vitamins C and E may bolster lens defenses, though definitive protocols are still pending.
- Monitor intra‑ocular pressure: Glaucoma often co‑exists with steroid‑induced cataracts; controlling pressure preserves optic nerve health.
- Educate patients: Clear communication about visual warning signs improves early reporting and reduces anxiety.
Comparison: Steroid‑Induced vs. Age‑Related Cataracts
| Feature | Steroid‑Induced Cataract (PSC) | Age‑Related Cataract |
|---|---|---|
| Typical Location | Posterior subcapsular region | Both cortical and nuclear zones |
| Onset Speed | Weeks to months after steroid exposure | Years, gradual progression |
| Common Symptoms | Glare, halos, near‑vision blur, color fading | General blurriness, difficulty with night driving |
| Risk Factors | High steroid dose, topical use, long duration | Age >60, diabetes, smoking, UV exposure |
| Prevention | Dose minimisation, regular eye exams | UV‑blocking sunglasses, diabetes control |
| Surgical Outcome | 92 % excellent visual recovery (London Cataract Centre) | Similar high success rates, slightly lower complication risk |
Practical Checklist for Patients on Steroids
- Ask your prescribing doctor for a baseline eye exam before starting long‑term steroids.
- Schedule follow‑up exams every 3‑4 months if you’re on high‑dose or topical therapy.
- Report any new glare, halo, or sudden blurriness immediately.
- Never taper or stop steroids without medical advice.
- Discuss steroid‑sparing alternatives if you have chronic inflammation.
- Keep a list of all steroid formulations you use (dose, route, frequency) for your eye doctor.
Frequently Asked Questions
Can a short course of steroids cause cataracts?
Short bursts (less than two weeks) rarely lead to visible PSCs. The risk climbs sharply after about four weeks of continuous use, especially at high doses.
Is cataract surgery safe for someone who must stay on steroids?
Yes, but surgeons schedule tighter post‑op follow‑up and may use additional anti‑inflammatory drops to keep the eye quiet while the IOL heals.
Do inhaled steroids for asthma count as a risk?
Inhaled steroids do contribute, though the risk is lower than with topical eye drops. The 2024 Al Ahsa study found only 38.6 % of inhaler users were aware of the cataract link.
Can antioxidants really protect my lens?
Early trials suggest vitamins C and E may reduce oxidative damage, but no official guidelines exist yet. Talk to your eye doctor before starting supplements.
What if I need steroids for a life‑threatening condition?
The benefit of controlling the primary disease usually outweighs the cataract risk. In such cases, doctors aim for the lowest effective dose and monitor the eyes closely.
Next Steps for Readers
If you’re currently on any form of corticosteroid, schedule an eye exam within the next month. Bring a list of every steroid you use, including over‑the‑counter inhalers or creams, so the ophthalmologist can assess your cumulative exposure. If you notice any of the visual changes described above, call your eye doctor right away-early intervention can keep you from needing surgery sooner than necessary.
For healthcare providers, incorporate a mandatory ophthalmic baseline check into your steroid prescribing workflow. Document dose, route, and expected duration in the patient’s chart; set reminders for follow‑up eye exams at three‑month intervals for high‑risk cases.
Ultimately, understanding the link between steroids and cataracts empowers both patients and clinicians to strike a balance: keep inflammation under control while preserving clear vision for years to come.

Cheyanne Moxley
October 25, 2025 AT 17:38People think steroids are harmless pills you can pop without consequences, but that’s a dangerous illusion. The reality is that we’ve all got a duty to question why doctors keep handing out high‑dose steroids without a warning label. When you’re on a medication that can cloud your vision, you should demand a baseline eye exam before even starting the treatment. Ignoring the risk is basically signing a consent form you never read. If we keep turning a blind eye to steroid‑induced cataracts, we’re complicit in a silent epidemic.
Take responsibility for your health and push for better patient education.
Kevin Stratton
November 10, 2025 AT 21:31Contemplating the balance between inflammation control and ocular clarity feels like an age‑old paradox :) The lens, a crystal of protein, reminds us that even the smallest molecular change can ripple into our perception of the world. Steroids, while taming fire, can also dim the very light that guides us. Imagine a world where every prescription comes with a built‑in reminder to check the eyes – that would be a true harmony of science and foresight. 📚
Manish Verma
November 27, 2025 AT 02:24In our great nation we pride ourselves on cutting‑edge medicine, yet we still let patients walk into clinics without a single glance at their eyes when they’re handed steroids. It’s a short‑sighted policy that betrays the very pride we claim to uphold. The data is clear: high‑dose topical steroids multiply the cataract risk several fold, and we shrug it off as “just a side effect.” Our doctors should act like true guardians of vision, not lazy by‑standers. By demanding routine slit‑lamp exams we reinforce the standards that make our healthcare system exemplary. Let’s stop the complacency and demand accountability across every prescription desk.
Lionel du Plessis
December 13, 2025 AT 07:18The ocular pharmacodynamics of topical glucocorticoids accelerate protein‑crosslinking via oxidative pathways resulting in posterior subcapsular opacity.
Andrae Powel
December 29, 2025 AT 12:11When you’re prescribed steroids, the first step isn’t just about the dosage, it’s about setting up a safety net for your eyes. A baseline slit‑lamp examination establishes a reference point so any future changes are easy to spot. Follow‑up visits every three to four months allow the ophthalmologist to catch the tiniest grayish specks before they grow into full‑blown cataracts. If the patient’s intra‑ocular pressure starts to creep up, it can be managed with pressure‑lowering drops, preventing a double whammy of cataract and glaucoma. Discussing the risk with your primary care physician ensures that both sides of the treatment plan are aligned. Lowering the steroid dose whenever feasible is a cornerstone of risk mitigation, and many clinicians now start with the lowest effective strength. For those who need long‑term therapy, swapping to steroid‑sparing agents such as biologics can dramatically cut down exposure. Antioxidant supplementation, while not officially recommended yet, shows promise in early trials and can be considered after consulting your eye doctor. Keeping a written log of every steroid product, including inhalers, creams, and eye drops, makes the conversation with your ophthalmologist much smoother. If any new glare, halo, or sudden blurriness appears, schedule an appointment immediately – early intervention often means the cataract is still small enough to monitor. The surgical outcomes for steroid‑induced PSCs are excellent when the lens is removed and an IOL implanted, but postoperative inflammation must be tightly controlled. Surgeons may prescribe additional anti‑inflammatory eye drops around the time of surgery to keep the eye quiet. Patients who cannot taper off steroids should be warned about the higher chance of posterior capsular opacification later on. Education is vital: many patients are unaware that even inhaled steroids carry a modest risk, so spreading this knowledge can prevent surprise vision loss. Finally, remember that the goal is to suppress the underlying disease without sacrificing clear vision, and with diligent monitoring, that balance is achievable.
Leanne Henderson
December 31, 2025 AT 19:44Wow, that was a thorough rundown! 🙌, I love how you broke everything down step‑by‑step, it really demystifies the whole process, and the reminder to keep a log? Genius! 🙏, staying proactive with eye exams can truly save us from a blurry future, and your point about antioxidants is so encouraging-maybe we should explore that together?, also, never underestimate the power of a supportive doctor‑patient partnership, because that trust makes all the difference!!!, keep spreading this valuable info, it’s a beacon for anyone on steroids.
Megan Dicochea
January 3, 2026 AT 03:18That philosophical angle hits home steroids can dim the light we see but also calm the fire inside it’s a balance we need to respect and monitor regularly.
Jennie Smith
January 5, 2026 AT 10:51Let’s turn that caution into action! 🌟 Imagine a world where every steroid prescription comes with a superhero‑style eye‑check badge-your vision stays sharp, your health stays strong. You’ve got the power to demand that extra exam, and together we can make it the new norm. Keep the conversation alive, keep those lenses clear, and watch confidence bloom like sunrise over a crystal lake.