Tick Fever Prevention and Treatment Outlook 2025
 Oct, 15 2025
Oct, 15 2025
Tick Exposure Risk Calculator
Tick Exposure Risk Assessment
Your Tick Exposure Risk Assessment
Based on your activity and precautions:
Key Takeaways
- Tick fever remains a growing concern as warmer climates expand tick habitats.
- Current prevention relies on personal protection and prompt tick removal; emerging tools include vaccines and gene‑edited tick control.
- Doxycycline is the frontline treatment, but resistance and side‑effects are driving research into new antibiotics and monoclonal antibodies.
- Rapid diagnostic PCR tests are shortening the time from bite to treatment, improving outcomes.
- Travelers and outdoor workers benefit from a simple checklist: check, repel, remove, and record.
Understanding Tick Fever
When we talk about tick fever is a collective term for several fever‑inducing illnesses transmitted by ticks, most commonly caused by bacteria such as Borrelia (responsible for relapsing fever) or Rickettsia (causing spotted fevers). The disease usually starts with a bite‑site rash, high temperature, and muscle aches, and if left untreated can lead to organ involvement.
Ticks themselves are tiny arachnids that attach to hosts for blood meals. A single tick can harbor multiple pathogens, making it a potent vector for a range of infections beyond fever, such as Lyme disease and anaplasmosis.
Current Prevention Strategies
Most public‑health guidelines focus on three pillars: avoidance, protection, and early removal.
- Habitat avoidance: Stay on clear paths, avoid tall grass, and perform a thorough skin check after any outdoor activity.
- Personal repellents: Products containing DEET (20‑30%) or picaridin (10‑20%) repel ticks effectively. Clothing treated with permethrin adds an extra barrier.
- Prompt removal: Use fine‑tipped tweezers to grasp the tick close to the skin, pull upward steadily, and disinfect the bite area.
While these steps are simple, compliance drops in hot weather when people wear short sleeves and shorts. That’s where emerging technologies aim to fill the gap.
Existing Treatment Landscape
The go‑to drug for most tick‑borne fevers is doxycycline. A 7‑day course resolves symptoms in 90% of cases and shortens fever duration by half. However, doxycycline can cause photosensitivity and upset stomach, which deters some patients.
For pregnant women or children under eight, alternatives like amoxicillin or ceftriaxone are used, though they are less effective against certain rickettsial strains.
Rapid diagnosis is crucial. Traditional serology can take weeks, but modern PCR tests can detect bacterial DNA within 24hours, allowing clinicians to start doxycycline sooner.
Emerging Prevention Innovations
Researchers are tackling tick fever from three angles: vaccines, tick‑population control, and digital surveillance.
| Measure | Stage | Mechanism | Key Benefits |
|---|---|---|---|
| DEET / Picaridin Repellents | Widely available | Skin‑applied chemicals that mask host odors | Immediate protection, low cost |
| Permethrin‑treated Clothing | Common in outdoor gear | Insecticide embedded in fabric fibers | Long‑lasting, protects covered skin |
| Tick‑bite Vaccine (candidate) | PhaseII trials (2024‑2025) | Induces antibodies against salivary proteins | Potentially eliminates need for repellents |
| Gene‑edited ticks | Laboratory proof‑of‑concept | CRISPR disables pathogen‑binding genes | Reduces disease transmission at source |
| AI‑driven habitat mapping | Pilot projects in Queensland | Satellite data predicts tick hotspots | Helps public‑health agencies target interventions |
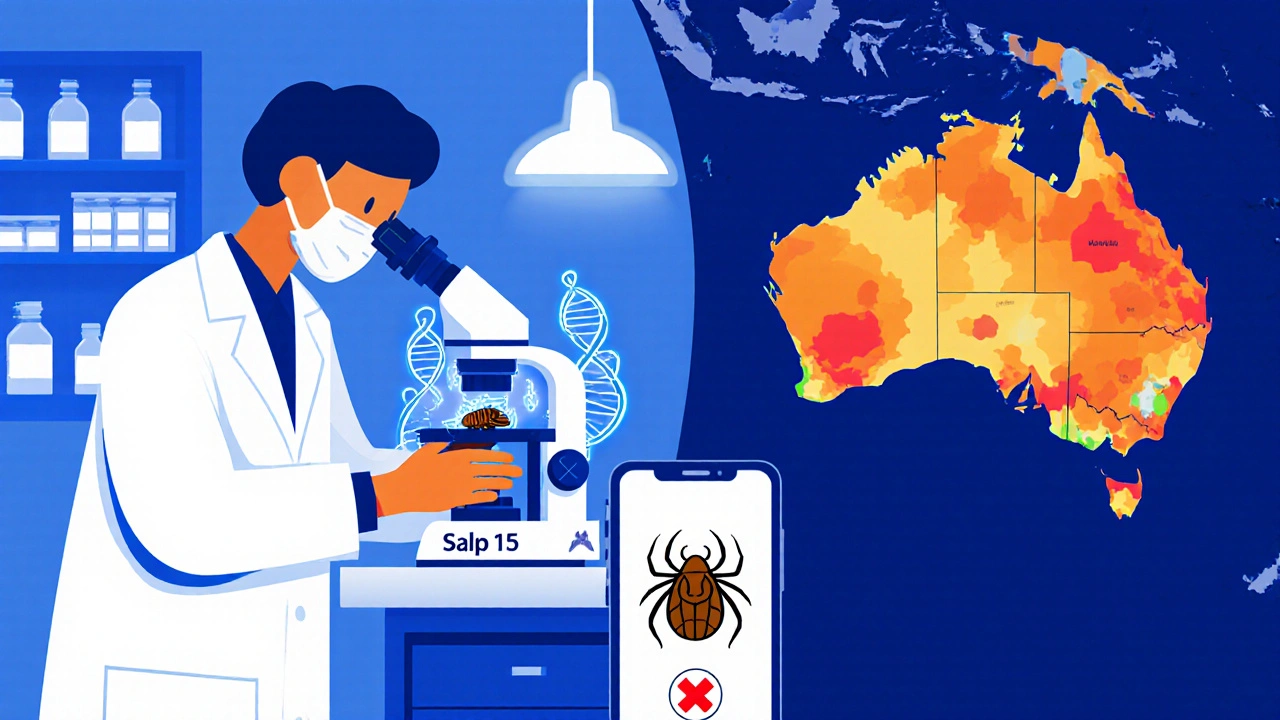
The most promising vaccine candidate targets the salivary protein “Salp15,” which ticks inject to suppress host immunity. Early trials show a 70% reduction in infection rates among vaccinated volunteers.
Gene‑editing ticks is still controversial-ethical concerns and ecological impact need thorough assessment-but the technique could eventually produce tick populations that cannot carry Borrelia or Rickettsia.
Future Therapeutic Developments
Beyond doxycycline, pharma companies are testing new drug classes:
- Novel tetracycline analogues with reduced photosensitivity.
- Monoclonal antibodies that neutralize the bacterial outer‑membrane proteins, offering a one‑dose therapy.
- Bacteriophage therapy targeting specific Borrelia strains, currently in animal models.
Another avenue is host‑modulation drugs that boost the immune response at the bite site, preventing the bacteria from establishing a foothold. Early-phase trials of a small‑molecule adjuvant showed faster fever resolution in a cohort of 120 patients.

Impact of Climate Change & Ecology
Warmer winters and milder summers in southern Australia have expanded the range of the tick species Ixodes holocyclus. A 2023 climate change model predicts a 30% increase in suitable habitat by 2035.
Consequences are two‑fold: more people are exposed, and the tick season lengthens from roughly 4months to 7months in Queensland. Public‑health agencies are therefore investing in community education and real‑time tick‑alert apps.
Practical Checklist for Travelers & Outdoor Workers
Use this short list before, during, and after outdoor activities:
- Apply DEET‑based repellent to exposed skin at least 30minutes before heading out.
- Wear permethrin‑treated pants and long‑sleeve shirts.
- Do a full‑body tick inspection every two hours; pay special attention to scalp, behind ears, and groin.
- If you find a tick, remove it with tweezers, disinfect the bite, and note the date.
- Monitor for fever, rash, or flu‑like symptoms for two weeks; seek medical care promptly if they appear.
- Consider prophylactic doxycycline (200mg) within 72hours of a high‑risk bite, after consulting a clinician.
Keeping a simple log on your phone helps clinicians decide whether a prophylactic dose is warranted.
Frequently Asked Questions
How quickly do symptoms appear after a tick bite?
Most people develop fever, headache, or a rash within 3‑7 days, but some infections can stay hidden for up to two weeks.
Is there a vaccine for tick fever yet?
A vaccine targeting the tick salivary protein Salp15 is in PhaseII trials as of 2025. It’s not commercially available, but early data look promising.
Can I treat a tick bite at home?
You can safely remove the tick and monitor for symptoms, but antibiotics should only be started after a healthcare professional confirms the need.
Do DEET repellents protect against all tick species?
DEET works on the majority of tick species, including Ixodes and Amblyomma. However, regular skin checks remain essential because no repellent offers 100% coverage.
What role does climate change play in tick fever risk?
Warmer temperatures expand tick habitats and lengthen the active season, leading to higher exposure rates and more cases of tick‑borne diseases.

Ryan Smith
October 15, 2025 AT 19:26Oh sure, just spray yourself in DEET and the ticks will obey.
John Carruth
October 21, 2025 AT 14:19Look, the article does a solid job laying out the basics, but let’s take a step back and think about how we actually implement these measures in the real world. First, personal repellents are great on paper, yet compliance drops dramatically during the heat of summer when people ditch long sleeves. Second, the checklist is useful, but without a community-driven reminder system, many hikers forget the two‑hour inspection rule. Third, the vaccine candidate looks promising, but we need to consider how quickly it can be rolled out to remote populations. Fourth, gene‑edited ticks raise ethical questions that aren’t addressed in the piece, and we should be wary of unintended ecological effects. Fifth, the AI habitat mapping could revolutionize public health, but only if agencies have the budget to act on those insights. Finally, education is the backbone – if we teach kids early about tick checks, we build lifelong habits that reduce disease incidence.
Melodi Young
October 27, 2025 AT 08:12Nice rundown, John. I’d add that while the checklist is handy, many people skip step three – the full‑body inspection – because they’re in a rush after a hike. Also, the article glosses over the fact that doxycycline can cause severe gut upset in some users, which pushes them towards alternative antibiotics even if they’re less effective.
Tanna Dunlap
November 2, 2025 AT 03:06The vaccine discussion feels too rosy. We need to ask who’s funding these trials and whether the data will be publicly available. Introducing a Salp15‑based vaccine without transparent safety monitoring could set a dangerous precedent. Moreover, gene‑editing ticks, while scientifically fascinating, skirts around the moral responsibility we have to ecosystems. If we start altering species for our convenience, where does it stop? The article should have highlighted these ethical dilemmas more prominently.
Troy Freund
November 7, 2025 AT 21:59Thinking about ticks always brings up the larger picture – we’re dealing with a complex web of climate, wildlife, and human behavior. The more we understand the tick’s role in the ecosystem, the better we can design interventions that don’t tip the balance. Simple habits like checking after a walk are small but powerful. When we combine those habits with smarter tech, we get a holistic defense.
Liam McDonald
November 13, 2025 AT 16:52Dear readers the article clearly outlines the current prevention methods the importance of personal protection as well as the emerging technologies such as vaccines and gene edited ticks The discussion on climate change impacts is also well presented however the piece could benefit from more detailed guidance on how to implement the checklist in varied environments especially for those living in high risk areas
william smith
November 19, 2025 AT 11:46Key takeaways: DEET and permethrin still work, check yourself often, and keep an eye on new vaccines. If you get a bite, see a doctor within 72 hours for possible prophylaxis.
Timothy Javins
November 25, 2025 AT 06:39Sure, the article says vaccines are coming, but who knows if they’ll ever be affordable for people in rural areas.
Kay Yang
December 1, 2025 AT 01:32Great summary! 👍 I love the practical checklist – it makes the science actionable. 🌿
Rajesh Kumar Batham
December 6, 2025 AT 20:26Exactly! A quick check after a hike can save you a lot of trouble. 😅👍
Bill Gallagher
December 12, 2025 AT 15:19First, let’s acknowledge that the article does a commendable job summarizing the current state of tick‑borne disease prevention, yet it falls short in a number of critical areas. Second, the reliance on doxycycline as the frontline therapy, while standard, is presented without sufficient discussion of the growing resistance patterns noted in recent surveillance data; this omission may mislead clinicians into a false sense of security. Third, the piece mentions the novel tetracycline analogues but fails to explain their mechanism of action, which, for the informed reader, is essential for understanding why they might reduce photosensitivity. Fourth, the discussion of monoclonal antibodies is overly optimistic; the clinical trials referenced are still in Phase I, and the article does not address the cost‑effectiveness concerns that accompany biologic therapies. Fifth, the vaccine candidate targeting Salp15 is indeed promising, but the article neglects to mention the need for adjuvant optimization to elicit a durable immune response in diverse populations. Sixth, gene‑edited ticks are introduced as a potential solution, yet the ecological impact assessments are barely touched upon, and the risk of horizontal gene transfer to non‑target species is a serious consideration. Seventh, AI‑driven habitat mapping is highlighted, but the piece does not discuss the data privacy implications of collecting geolocation data from mobile users. Eighth, the checklist is useful, but it does not account for occupational exposure scenarios where workers may be unable to perform self‑checks during active duty. Ninth, climate change is identified as a driver of expanded tick habitats, but the article could have provided more granular predictions, such as regional shifts in Ixodes holocyclus distribution over the next decade. Tenth, the reference to prophylactic doxycycline within 72 hours is accurate, yet the article omits the contraindications for pregnant women and children, which are paramount for safe prescribing. Eleventh, there is no mention of alternative repellent formulations like IR3535, which have been shown to be effective and may be preferable for individuals with skin sensitivities to DEET. Twelfth, the rapid PCR diagnostic tools are praised, but the potential for false‑positive results due to contamination is not addressed, a point that laboratories must vigilantly monitor. Thirteenth, the article could improve by integrating a discussion of public health policy, such as funding for community tick‑surveillance programs, which are essential for early detection of emerging hotspots. Fourteenth, the role of citizen science platforms, where the public contributes tick sighting data, is absent, despite their growing influence in epidemiological modeling. Fifteenth, finally, the article would benefit from a more balanced view on the ethical considerations surrounding gene editing and vaccine rollout to ensure that scientific advancement proceeds responsibly.
Rajashree Varma
December 18, 2025 AT 10:12Wow, that was a thorough deep‑dive, Bill. It’s reassuring to see such a balanced perspective that acknowledges both the promise and the pitfalls of new technologies. The emphasis on ethics and cost‑effectiveness really grounds the discussion in real‑world concerns.
Anshuman Pandey
December 24, 2025 AT 05:06From a philosophical standpoint, the tug‑of‑war between human intervention and natural processes is evident here. Our attempts to control tick populations mirror broader attempts to dominate nature, raising questions about long‑term sustainability. Yet, with climate change accelerating, some level of intervention may become unavoidable. The key is to proceed with humility, guided by rigorous data and ethical reflection.
Thomas Malloy
December 29, 2025 AT 23:59Check early, stay safe.
Sushma Gowda
January 4, 2026 AT 18:52That’s a solid mantra, Thomas. Remember to also keep your gear clean; a quick wash after a hike can remove any stray ticks that might have clung to fabric. Consistency is the secret sauce for staying tick‑free.
Angie Wallace
January 10, 2026 AT 13:46Good point. Education and simple habits go a long way.
Doris Montgomery
January 16, 2026 AT 08:39Too much hype, not enough real‑world data. The checklist sounds nice, but it’s not a magic bullet.